
Prolotherapy; A revolutionary treatment that has given the gift of a pain-free life to many across the globe. But what exactly is Prolotherapy? How does it work? Is it truly a regenerative treatment as many clinicians claim?
Let’s discuss the research and findings that suggest that Prolotherapy can be used as an alternative, non-surgical solution for musculoskeletal problems.
What is Prolotherapy?
Prolotherapy, in simple words, is a non-surgical regenerative medicine technique that involves injecting a sclerosant solution, to an area of the body which may be damaged or show degeneration.
This deliberate irritation using a specially formulated Prolotherapy solution, stimulates the body’s natural healing mechanism, which in turn helps regenerate and rejuvenate the surrounding tissues, ligaments, tendons, and cartilage.
Your physician will recommend multiple treatment sessions to promote and facilitate the growth and regeneration of cells and tissues.
The sclerosing solution, is normally a solution of concentrated Dextrose.
In the lower back, we also use a Solution known as P2G which is abbreviated for Phenol-Glycerin-Glucose.
Research has shown this has a role in Cartilage Cell Regeneration (Johnston et al, 2020)
Prolotherapy comes under the banner of Regenerative medicine, as it shares similarities with stem cell treatments and tissue engineering.
The remarkable aspect of Prolotherapy is that it can help rejuvenate degenerating joints and tissues without requiring stem cells.
Numerous studies have shown positive results in patients with knee arthritis or tendinopathies and other musculoskeletal issues.
Post-treatment, patient prognosis has been good, with improved strength and function, reduced stiffness and pain in joints, followed a more mobile lifestyle than before.
This treatment modality uses your body’s own healing response to switch on the healing process.
The ligaments and tendons that form after the treatment appear to be much like normal tissue, with additional strength and thickness, indicating the growth of healthy tissue.
Prolotherapy is a non-surgical intervention that can be quickly done as an in-office procedure.
It is now a mainstream treatment and is practised all over the world in several countries
Let’s take a look at the most commonly treated regions by Prolotherapy:
1. Prolotherapy: Neck Pain/ Strain

In our increasingly digital world, using cell phones and long hours at the desk with sedentary jobs have resulted in multiple ailments primarily centred around the head and neck region.
A recent study indicated that neck pain is one of the most common musculoskeletal disorders.
Acute neck pain affects up to 70% of the population. However, chronic neck pain can persist for extended periods and this can become very problematic in the long term.
Currently, conventional treatments include either Cortisone or medications such as Gabpanrtin or Codeine with numerous side effects such as Nausea or Sedation.
It is important to mention that there is no quick fix that can treat all neck pain or stiffness. Each case needs to be treated individually on a case by case basis.
Chronic neck pain can be due to whiplash injury or cervical degeneration including Disc herniation or Arthritis causing instability. This often requires a thorough examination or Xray/MRI and additional imaging to determine the underlying cause.
Cervical instability due to related damage to ligaments in the cervical spine, should rely on a treatment focusing on strengthening the ligaments in the neck region.

How can Prolotherapy help?
Prolotherapy is an intervention that can turn your life around and help you regain control if you have been suffering from chronic pain.
The treatment is used for acute and chronic musculoskeletal conditions, such as those that cause chronic neck pain due to ligament laxity and joint instability.
Doctors are faced with a predicament while treating capsular ligament laxity since ligaments have an absent blood supply, which ultimately impairs healing. Conventional treatments do not address this issue, so the long-term prognosis is often poor.
The mechanism for prolotherapy treatment is based on 3 principles:
1. Inflammation
2. Remodelling
3. Proliferation
These three stages result in a regenerative healing process that ultimately provides us with the results we need.
Prolotherapy results in a healing response at the injection site and triggers a similar response in the surrounding structures, such as tendons and ligaments.
One of the pioneers of Prolotherapy, George Hackett, MD, developed the technique in the 1950s.
The technique, to date, has been used to treat countless patients exhibiting whiplash injuries. For instance, Hackett et al (1962) and his team discovered that more than 85% of patients with a cervical ligament injury had no symptoms of Whiplash Associated Disorder or headaches once Prolotherapy was administered.
Barre- Lieou Syndrome:
A common occurrence that results from ligament laxity and instability is the Barre-Lieou syndrome. The syndrome is named after the two doctors who discovered and observed it in the early 1900s.
A whiplash injury or continuous long-term pain in the neck, ultimately creates space between the ligaments of the neck.
What’s interesting to note is that, most physicians misdiagnose the condition since it cannot be detected on an MRI and is only noted upon careful physical examination, particularly observing the neck in motion. The syndrome has caused a fair share of controversy due to this reason.
In simple words, the condition signifies the deterioration of the vertebrae bones that occurs over time ; the ligaments holding the bones together over-stretch causing instability in the neck.
As the neck becomes more and more unstable, the nerves of the neck become chronically irritated, which results in many uncomfortable symptoms such as ringing in the ears, headache, dizziness, fogginess and allergy-like symptoms.
Prolotherapy has been effective in relieving these symptoms, in even the most severe of cases.
Let’s take a closer look at some evidence-based studies:
CASE STUDIES
Cervical Instability as a cause of Barre-Lieou syndrome: A case series
Between 2011 – 2013 , eight patients with Barre-Lieou syndrome were treated for chronic neck pain symptoms that they had been experiencing since the trauma.
All patients reported improvement of neck pain and associated symptoms with increased physical activity. The patients reported a significant decrease in crepitation (neck popping,cracking and grinding noise) as well as forgoing the need to use a soft collar altogether. Hauser et. al (2015) concluded that prolotherapy should be considered a treatment option for patients with Barre-Lieou syndrome.
Why does Prolotherapy work in the neck:
Since one of the the underlying causes of cervical instability is laxity of the cervical ligaments and vertebrae, prolotherapy strengthens the ligaments over time.
As the ligaments become stronger, they act as a ‘brace’ around the bones in the neck and reduce instability.
This relieves pressure on the sympathetic nervous system, thereby relieving the patient of the symptoms that they were experiencing.
Cervical Capsular Ligament Injuries following Whiplash injury : A Case series
Capsular ligaments hold a stabilising position within the facet joints (Zypophyseal joints) and have been observed to be a major factor in chronic neck pain for patients. When these joints are injured, following a neck injury or whiplash injury, they tend to become stretched and elongated.
This results in laxity and excessive movement of the cervical vertebrae. These spinal ligaments interconnect each facet joint together and following an injury, they may cause abnormal motion. Most clinicians may struggle to diagnose this as it is not always clear on imaging such as Xray or other scans.
Let’s take a look at these ligaments:


It can be observed that the cervical capsular ligament, as shown in figure 1, is extremely small and thin. This ligament is prone to getting injured in spinal trauma and tends to be the most overlooked one.
It is important to note that prolotherapy not only treats joints, but also the tendon and ligament attachments that surround them; as a result, it is a comprehensive and highly effective method of wound healing and pain relief. The capsular ligaments are the main stabilising structures of the cervical spine’s facet joints (Figure 2) and have been linked to chronic neck pain.
When the capsular ligaments are injured, they become elongated and lax, causing the cervical vertebrae to move excessively. This can cause symptoms such as nerve irritation and vertebrobasilar insufficiency in the upper cervical spine (C0-C2), as well as vertigo, tinnitus, dizziness, facial pain, arm pain, and migraine headaches.
In addition to chronic neck pain, this can also cause muscle spasms, crepitation, and/or paresthesia (numbness and pins and needles in the lower cervical spine (C3-C7).
Prolotherapy is an effective treatment for chronic neck pain and cervical instability, particularly when caused by ligament laxity. The technique is both safe and non-invasive, as well as effective in treating chronic neck pain and its associated symptoms.
Prolotherapy for recurring headaches and migraine pain : A Case study
An astonishing 86 million workdays are lost annually to migraines in the UK, as stated by this study here.
An estimate by the Global Burden of Disease 2016 found that 23.3% of adults are affected by migraines in the UK.
Research has tried to establish a connection between a weakness in the cervical ligaments and recurring headaches/migraines and administering Dextrose prolotherapy which would ultimately relieve the patients pain.
Conventional treatment includes the use of muscle relaxants, NSAIDs and triptans. Despite all these interventions, only 50% of patients describe a reduction in the occurrence of migraine and headaches after three months of treatment.
A study was conducted between 2001 – 2005, in a Christian Charity medical clinic in Southern Illinois consisting of 15 patients by Hauser et.al (2009).
Each patient was given dextrose solution mixed with lidocaine (15% Dextrose + 0.2% Lidocaine) at specific marked points in the head and neck region.
Before the treatment 54% reported tension headaches, while 46% were suffering from migraine headaches, prior to prolotherapy treatment. 34% of the patients reported daily headaches with 80% experiencing headaches at least once a week.
Data was collected, precisely 22 months after the last prolotherapy treatment.
After prolotherapy treatment, 60% of the patients reported a reduction in the occurrence of painful headaches, down to once per month.
All participants stated a decrease in the level of pain, with just one patient continuing to have headaches on a daily basis. Additionally, 47% of patients stated that their pain intensity level was close to zero after receiving treatment. 73% of patients also reported a decrease in sensitivity to light during a headache episode, while overall, symptoms that are associated with tension and migraine headaches were decreased in 80% of the patients participating in the study.
2. Shoulder Rotator Cuff Tears
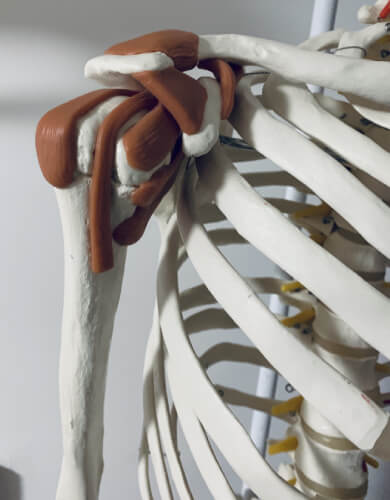
The shoulder joint has a complex anatomy, which exhibits a wide range of motion that allows us to be mobile. More specifically, the shoulder has a group of muscles and tendons called the rotator cuff, which forms a ‘cuff’ like structure together over the shoulder.
In many cases, rotator cuff tears are a major reason for chronic shoulder pain.
This usually results from joint overuse in both office workers and those who do much manual labour work. The repetitive overuse of the shoulder can result in tendinopathy and eventually tiny tears in the rotator cuff muscles.
This can lead to chronic pain that the patient feels as slowly, with time and ageing, degeneration begins to settle in.
Numerous studies indicate that patients suffering from shoulder rotator cuff tears can benefit from Prolotherapy. For example, M.M Seven et. al (2017) found that out of 101 patients, 53 patients reported an improvement side-by-side with a good home exercise program.
Rotator cuff tendinopathy is the leading cause of shoulder pain amongst all age groups. The shoulder joint is a mobile joint and an equally unstable one too.
Conventional therapies suggest active rest, physical therapy, ibuprofen, and corticosteroid injections, but none of these treatments address the underlying cause – ligament degeneration and laxity.
Prolotherapy injections have been found to have beneficial effects as they help shorten the patient’s rehabilitation time while addressing the underlying cause.
Additionally, the injections have been found to propagate healing by stimulating the extracellular matrix, which in turn helps increase the joint’s stability by strengthening the tendons and ligaments.
CASE STUDIES
Lets Compare Prolotherapy to Cortisone and PRP in treating Rotator Cuff Tears
Dextrose prolotherapy, Platelet-rich plasma or Corticosteroid injections : A Case study for Rotator Cuff Tendinopathy
Rotator Cuff Tendinopathy of Rotator Cuff Disease is one of the leading causes of shoulder disability.
Conservative treatment suggests the use of NSAIDS, physical manipulation, and physiotherapy. These do not always relieve pain in the long run.
Many patients seek alternative therapies such as prolotherapy and platelet-rich plasma which we will look at closely in this study.
Prolotherapy consists of injecting an irritant, such as dextrose solution, at a site where the patient is experiencing pain. Platelet-rich plasma involves using the patient’s own centrifuged blood and reinjecting it back into the body. This centrifuged blood is rich in cytokines, platelets, and multiple growth factors. The platelet-rich plasma is thought to help in the regeneration of cells in the area that it is injected into.
Lastly, corticosteroids are strong anti-inflammatory drugs that provide pain relief, upon injection.
Sabaah and Nassif et.al (2020) studied Rotator Cuff Tendinopathy, over the course of one year, consisting of 60 patients with Rotator Cuff Tendinopathy (RCT). These patients had been diagnosed clinically with symptoms persisting for at least 3 months, and with failed conventional treatment.
A visual analog scale was used, (VAS) with a 0-10 scale that indicated 10 being the worst pain. The Visual Analog Scale was introduced by Patterson and Hayes in 1921. The scale is used in clinical research to measure the frequency of varying symptoms.
Another index called the WORC (Western Ontario Rotator Cuff) index is a quality of life evaluation questionnaire meant for patients afflicted with rotator cuff disorders.
In the study, the WORC index was used to evaluate the quality of life of the patients between 0 to 2100 with 0 meaning no reduction in the quality of life and 2100 indicating a bad score.
Patients were divided into three groups, one was given a Prolotherapy solution (dextrose), one was injected with PRP solution and the third was administered Cortisone injections.
Post injection, patients were instructed to keep their shoulder movement as limited as possible, for at least 48 hours. They could take paracetamol for pain but no NSAIDS.
Patients were recalled after three months and reassessed.
On reassessment, group 1 (prolotherapy) showed the best overall improvement, more than group 2 and 3.
Prolotherapy indicated the most improvement in VAS (Visual Analog Scale), WORC (Western Ontaro Rotator Cuff) index and mobility as well as in rotator cuff healing.
The study found that PRP injections also improved the WORC index to an extent coupled with tendon healing, however Cortisone injections had no effect on healing, whatsoever.
Prolotherapy was the clear winner here, more than PRP and conventional steroids.
Effectiveness of Prolotherapy in the treatment of Rotator Cuff Lesions
This study aimed to observe the direct results of Prolotherapy in the treatment of chronic rotator cuff lesions.
Seven et al (2017) observed 120 patients with rotator cuff lesion injury and with persisting symptoms for six months. Patients were divided in two groups; one was treated with prolotherapy, while the other were treated with only physiotherapy sessions, three times a week for 12 weeks. Both groups were told to follow a home exercise program.
Results obtained indicated that 53 patients in the prolotherapy group reported excellent outcomes, with significant improvement in shoulder motion at 3 weeks of treatment as compared to before.

3. Knee ligament injuries
Most knee ligament injuries initiate from fall or direct impact on the joint. With time, if the damage goes undetected, the joint exhibits obvious symptoms like increased stiffness and swelling.
If left untreated, knee instability can further lead to different chronic conditions such as:
-
- Knee Osteoarthritis
-
- Iliotibial band syndrome
-
- Runner’s knee
-
- Osteochondral defects
-
- Chondromalacia patella
-
- Patellar tendinitis
-
- Meniscus tears
The instability of the joint is caused by the weakness of the surrounding structures, such as the ligaments and tendons. If these ligaments and tendons are strengthened, they will help stabilise the joint significantly.
Prolotherapy treatment can help restore joint functions and halt degeneration in the long run. However,chronic ligament injuries may progress into knee arthritis, which we will explore further in the article.
CASE STUDIES
Knee Prolotherapy
Repair of a complete anterior cruciate tear using prolotherapy: a case report
This report aims to discuss a case, where a young 18-year old patient sustained a knee injury while on a skiing trip.
She had an unstable walk, was unable to climb stairs, and had more than 1 cm anterior drawer test.
The young patient decided to take prolotherapy sessions, 7 in number, over the next 15 weeks. After her third prolotherapy session, a home exercise routine was added to her routine.
The results were impressive. Grote W et.al (2009) stated that after 4 weeks, the patient was able to walk on a flat surface. After 12 weeks, she was able to ride a stationary bicycle for 30 minutes. At 15 weeks, the patient was able to climb stairs on her own and an MRI showed that the ACL was intact with distinct fibrosis.
The study concluded that Prolotherapy could successfully be used as an alternate therapy modality, on carefully selected patients. In this case it appears the ACL was likely strained rather than a total rupture
With total ACL rupture we recommend surgery with Prolotherapy an add on option when required for the surrounding structures. This is because the ‘Tibial shift’ can cause early degeneration in the knee meniscus and breakdown of Knee Cartilage
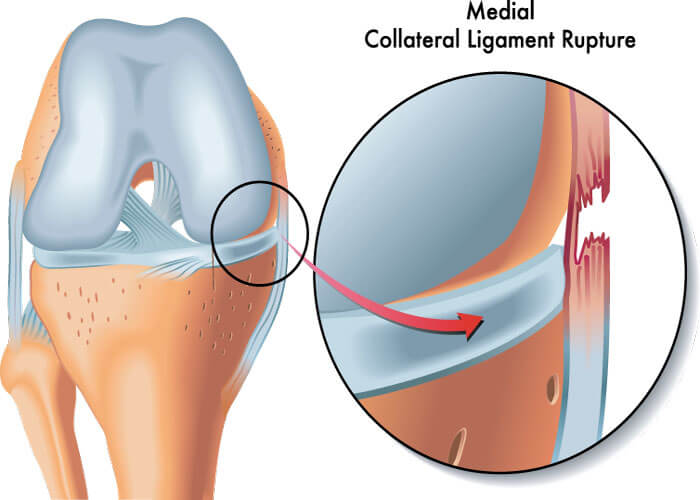
Treatment of a medial collateral ligament sprain using prolotherapy
A rugby player, with a grade 2 sprain of the MCL, was given Dextrose prolotherapy injections over the course of three weeks, combined with an exercise protocol. Adam et.al (2015) noted that at the end of three weeks, the patient had complete range of motion and was pain-free, able to resume all rugby related activities.
4. Prolotherapy for Knee Arthritis
Since the 1970s, researchers have observed a close relationship between ligament injuries that develop into knee instability and Osteoarthritis.
Over the course of 25 years, Eric L Radin et.al (1974) observed that ligament degeneration with time does result in OA. Physicians noticed that at the beginning of the study, the patients had stable joints, which slowly, over time, began to show signs of ligament weakness.
This led to the researchers concluding that ligament weakness is one of the causative factors leading to OA. It was also noted that the more severe the injury, the more severe the onset of Osteoarthritis.
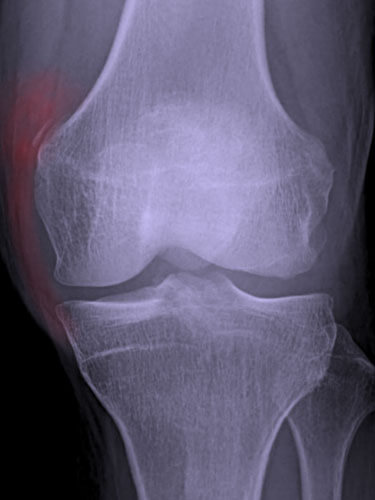
OA is diagnosed via an X-ray, with tell-tale signs of bony deposits distinguishable on film. OA progresses further and results in restriction of movement and pain for the patient. The bony deposits continue accumulating, ultimately obstructing and breaking down the protective cartilage layer in the knee joint.
The cartilage is a cushion of sorts, bearing the weight on the joint and keeping everything easy and soft within the joint.
With time, OA in the joint ultimately leads to degeneration.
OA is commonly seen in athletes and weightlifters and bodybuilders, as stated by Driban JB et.al (2017). This indicates that unresolved traumatic injuries and load-bearing activities accelerate the progression of degeneration.
CASE STUDIES
Dextrose Prolotherapy for Knee Osteoarthritis
Knee arthritis is a debilitating condition that results in stiff joints, pain and overall decreased function. A randomised controlled trial was conducted in order to evaluate and assess the efficacy of prolotherapy for osteoarthritis for the knees. Ragabo D et.al studied 90 participants, who had been suffering from knee osteoarthritis for at least three months prior to the study.
The patients were exposed to a random blind trial, where some patients were given placebo saline injections while the others received dextrose prolotherapy. The 3rd group of patients only adhered to at-home exercises throughout the tenure of the study.
Once the results were in, it was deduced that patients who received Dextrose prolotherapy showed great improvement while their individual knee pain scores also increased positively. The conclusion was drawn that Prolotherapy can show positive results in terms of pain, stiffness and function in osteoarthritis of the knee.
Prolotherapy for Knee Pain: A Case Series
Case 2
The first case by Alderman D, 2007 focuses on a young, 14-year old boy with anterior knee pain for one year after participating in a variety of sports for many years, including basketball, football, soccer, and baseball.
There was no prior trauma. He claimed to have been diagnosed with Osgood-Schlatter disease and was told there was nothing that could be done.
The patient experienced pain usually in the mornings, which lasted throughout the day and prevented him from participating in his usual activities and sports. As a result, he discontinued all athletic activities and was no longer involved in any sport, despite still experiencing daily pain.
On physical examination it was noted that there was Tibial tuberosity enlargement with tenderness to palpation at the patellar tendon insertion on the tuberosity on both sides, with no other anomaly reported.
The patient was prescribed three treatments to the left knee at three to four week intervals, while the right knee was given treatment once. The patient reported feeling 95-100% better in both knees and being able to resume full sports activity. He claimed that he could now “do anything.” After one – two years, there was stable improvement with continued full return to all sports.
5. Prolotherapy for Knee Meniscus tears
Our knees bear the weight of the entire body and the knee joint is the largest joint in the body. It’s also one of the most complex joints of the body.
The most common knee injuries in adults and children alike are ligament injuries. The second most common injury is a meniscal tear, which can be incredibly painful.
Meniscal injuries are the most common cause of knee pain. The damage is either caused by direct traumatic factors or meniscus degeneration due to ageing and wear and tear (also known as Degenerative Meniscus). First, let’s take a look at the anatomy of the knee:
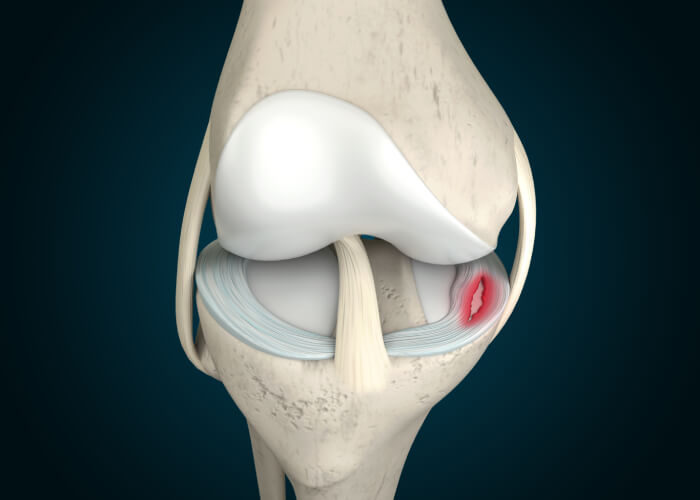
As you can see, the meniscus is a C-shaped structure that cushions the knee.
The medial meniscus is attached to the medial collateral ligament (MCL), an essential ligament that contributes to the overall stability of the joint.
Any injury to the medial meniscus will ultimately result in injury to the MCL. Instead, the meniscus gets operated on without addressing the underlying MCL sprain or injury, and the patient returns complaining of pain despite the meniscus surgery.
Traditional treatment VS Prolotherapy
We will look at the current treatment modalities that help patients with knee pain. Patients with meniscal tears are sometimes recommended surgery that involves removing a section or all of the meniscus. However, there is mounting evidence that surgery tends not to be successful in many cases.
The reason for this is simple; the meniscus tissue if removed also reduces the ‘shock absorbing’ capacity of the knee. Within 3-4 years we can have ‘bone contacting bone’.
Unfortunately when the medial meniscus deteriorates, it leads to the MCL becoming ‘lax’ too. With this in mind, it’s best to seek non-surgical interventions at first sight of knee pain to address the underlying cause well before time.
Prolotherapy and other treatments like Stem Cell Therapy have shown promising results.
Utilising either Dextrose Prolotherapy, physicians have been able to treat ligament injuries, thereby improving the overall laxity of the affected ligament over time.
CASE STUDY
The Case for Utilising Prolotherapy as First-Line Treatment for Meniscal Pathology
Knee meniscal injuries are one of the most common knee injuries to occur. Most meniscal tears are deemed to be too severe and lead the patient directly down the road to surgery.
Doctors and physicians have been investigating mechanisms to stimulate the repair of the meniscus,something which is rarely seen in surgical interventions.
Surgery involves partial meniscectomy, meniscus transplantation and to some degree meniscus repair as well, but the prognosis 5 years post surgery is not always successful.
Most patients return with recurring symptoms like re-injury, pain, instability and locking of the joint. In the long-run, the joint begins to internally degenerate, posing further risk for injury and deterioration of the patients health.
Since the damaged meniscus lacks a blood supply, it becomes difficult trying to initiate any kind of healing. Studies have found that growth factors can actually increase collagen growth and meniscus cell proliferation. Hence, prolotherapy can be used as a first line of treatment in select cases.
Hauser et.al (2010) carried out a study that involved twenty-four patients, who were suffering from meniscal injuries. The patients were called in for six prolotherapy sessions, with follow-ups taking place18 months after the last session.
It was found that prolotherapy greatly reduced patients knee stiffness and pain. Moreover, there was a significant improvement in walking ability, increased notable range of motion and crepitation as well as exercise.
6)Tendinosis
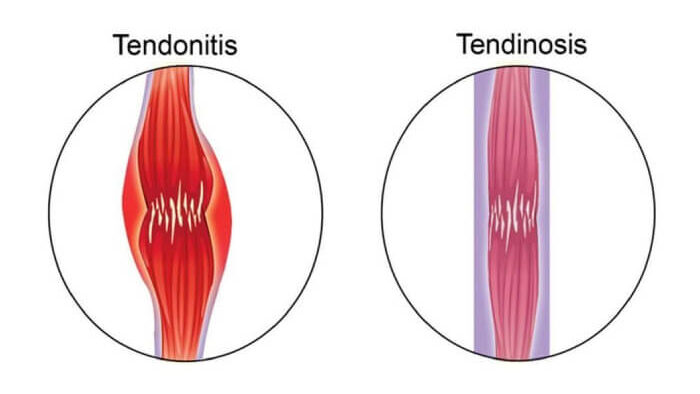
Tendinosis refers to the degeneration and breakdown of vital collagen in the tendon tissue. This results in the weakening of the connective tissue and pain when the tendon is used.
Prolotherapy helps by reversing the degeneration process to turn ‘on’ the body’s healing cascade. This will result in the repair and healing of the tendons as the dextrose solution prompts the body to release growth-factor elements at the injection site.
Prolotherapy has successfully treated four tendon disorders: hip adductor tendinopathy, Achilles tendinopathies, plantar fasciitis, and the patella tendinopathy.
CASE STUDIES
Prolotherapy in Primary Care Practice
In Tendinosis histopathological examination has revealed the tendons to be frayed and thin, and sometimes severely damaged.
A common injury seen in athletes is the Achilles tendinopathy. A case series was carried out by Rabago D et al, (2010) where 36 individuals with the condition were given prolotherapy injections at six week intervals.
At 52 weeks, the patients reported that there was a decrease in pain severity by 88% during rest, 84% during regular activity and 78% during sports-led activities. Overall tendon thickness also decreased notably.
Comparative Effectiveness of Ultrasound-Guided Intratendinous Prolotherapy Injection with Conventional Treatment to Treat Focal Supraspinatus Tendinosis
Twelve patients with focal Supraspinatus tendinosis (the most common Rotator Cuff Muscle injury) were included in this clinical study carried out by George et.al (2018). The patients had previous unsatisfactory results, having gone through physiotherapy sessions one month earlier. Seven patients underwent prolotherapy sessions while five patients continued with standard physiotherapy, like before.
When the results were in, it was noted that the prolotherapy group had an improvement in shoulder abduction with better sleep scores as well. The trial concluded with the observation that ultrasound guided intratendinous prolotherapy injections improved patient shoulder abduction with better sleep within 12 weeks of treatment, when compared to conventional physiotherapy management.
7. Prolotherapy for Tennis Elbow
The elbow joint serves as a hinge, allowing the arm a range of motion. Here are some of the symptoms of elbow joint pain:
-
- Finger numbness
-
- Loss of range and motion
-
- Radiating pain in the forearm
-
- Crepitation on movement
-
- Weakened arm muscles
Prolotherapy can all help slow down the degeneration process in the elbow joint.
Our Prolotherapy treatments will heal and treat conditions such as Tennis and Golfer’s elbow. Kehribar L et.al (2021) observed that 37 patients suffering from chronic lateral epicondylitis improved remarkably following prolotherapy treatment.

CASE STUDIES
Prolotherapy in Primary Care Practice
Lateral epicondylosis (also known commonly as ‘Tennis Elbow’, is a highly prevalent condition.
Individuals who indulge in activities that load the upper body are most prone to developing the condition, especially athletes. Rabago D et.al (2010) carried out a study to find out if prolotherapy could help patients with elbow pain. The study also focused on determining the grip and extension strength in patients with chronic Lateral epicondylitis.
The author chose twenty patients, who were suffering from the ailment since the past six months, with no respite from using NSAIDs, rest and corticosteroid injections. They were
administered Prolotherapy injections in a randomised trial with a control group that was given injections with normal saline too .
Three Prolotherapy sessions were done, with the group receiving prolotherapy reporting decreased pain scores at 8 and 12 weeks. The control group did not report any notable changes. In fact, patients subjected to prolotherapy showed increased grip and isometric strength.The improvements seen in the patients were maintained at 52 weeks.
Favorable Outcomes After Sonographically Guided Intratendinous Injection of Hyperosmolar Dextrose for Chronic Insertional and Midportion Achilles Tendinosis
Ryan M et.al (2010) focused on patients with Achilles tendinosis, who were given dextrose injections under imaging. The study included 108 tendons (86 midportion and 22 insertional) from 99 individuals who had discomfort at the insertion or mid portion of the Achilles tendon for longer than 6 months. Before injecting a 25% dextrose-lidocaine solution into the tendon with a 27-gauge needle, grey-scale (5-12 and 7-15 MHz) and color Doppler sonography exams were performed. Each tendon’s structural characteristics and the presence of neovascularity were observed. Items from the VAS were noted at the baseline, posttest, and 28.6 months of follow-up.
Each patient required an average of five injection appointments, spaced 5 weeks apart apart (range, 1–13). From baseline to follow-up, there was a significant decrease in pain scores for both midportion, activities of daily living, and sport. Intratendinous rips and hypoechoic areas both shrank in size and severity, while neovascularity improved.

With strong long-term evidence, dextrose injections seem to offer a low-cost, safe therapy option for easing discomfort caused by disease at either the insertion or mid portion of the Achilles tendon.
8. Prolotherapy Plantar Fasciitis
Plantar Fasciitis is a fairly common injury in athletes and the general population.
Patients usually complain of pain along the soles of their feet, especially the foot arch.
Some symptoms of the condition are:
Heel Pain (first thing in the morning)
-
- Abnormal walk as the heel is offloaded
-
- Cramping of the foot arch
-
- Tingling and numbness sensation in the sole
Patients usually complain of pain that’s worse in the morning and slowly subsides during the day.
If we examine the foot’s anatomy closely, the heel is connected to the toes by the plantar fascia. Usually, whenever the fascia undergoes strain or wear and tear, it becomes swollen and inflamed, and it is referred to as ‘Plantar Fasciitis. As a result, the patient will often complain of achy but, at times, sharp pain, with stiffness around the heel area.
Prolotherapy is an excellent, non-surgical treatment modality for patients with plantar fasciitis. These chronic conditions arise due to ligament laxity, which Prolotherapy and other regenerative treatments address. Once the ligaments slowly begin to strengthen, the joints become more assertive, and the patient’s complaint is resolved.

Several studies have depicted the long-term beneficial effects of Prolotherapy. A study found that Dextrose therapy is a safe and effective treatment for patients with plantar fasciitis.
CASE STUDIES
Prolotherapy in Primary Care Practice
Plantar fasciitis is another fairly common injury in the world of sports. Slattengren A et.al (2010) conducted a study where patients with chronic plantar fasciitis were given prolotherapy injections over a duration of 21 months, at 6 week intervals. Pain scores were noted at baseline and 11.8 months and it was observed that pain scores were seen to improve during various activities and at rest.
A randomised-controlled trial of prolotherapy injections in the treatment of plantar fasciitis
The purpose of this study by Ersen et.al (2017) is to assess the effectiveness of prolotherapy injections in treating plantar fasciitis.
60 individuals with symptomatic persistent plantar fasciitis were allocated into control and prolotherapy groups at random during the months of October 2014 and October 2015.
Three times every 21 days, ultrasound guidance was used to administer prolotherapy injections into the plantar fascia, up to five separate locations. Three times per week for three months, patients in the control group were given instructions for stretching the plantar fascia and Achilles tendon. All patients received heel lifts as well as instructions to avoid heavy loading activities. At baseline and at the follow-up intervals of 21, 42, 90, and 360 days, the patients were assessed using the Visual Analog Scale (VAS), Food and Ankle Outcome Score (FAOS), and Foot Function Index (FFI).
50 patients in total completed the follow-up (26 patients in the prolotherapy group and 24 patients in the control group). At 21 days into treatment, there were no statistically significant changes between the groups in the pain and functional scores. At 42, 90, and 360 days after starting treatment, the prolotherapy group’s VAS and FAOS ratings were greater than those of the control group. By 42 and 90 days into the treatment, the prolotherapy group’s FFI scores were likewise higher than those of the controls; however, at 360 days, the values were comparable between the two groups.
We can deduce from the study that prolotherapy is a valuable adjunct therapy for treating chronic plantar fasciitis.
9. Prolotherapy for Lower Back Pain
Lower back pain is one of the most common reasons why patients visit a physician. Most recurring episodes are debilitating in nature and even progress into chronic states. Currently, 1/3rd of the UK adult population is affected by back pain each year.
While disc herniation is frequently cited as the source of pain, ligament injury is a more common cause of low back pain because spinal ligament laxity may precedes disc herniations.
MRI and CT scans are not unable to denote a ligament injury, unless it’s really severe.
Furthermore, as previously stated, MRI scans necessitate that the patient remain still. Small ligament or tendon abnormalities, on the other hand, may not show up on imaging until the joint is moving, so an MRI may miss the problem.
This simply means that radiographic findings should not always be accepted as the cause of pain until other sources have been ruled out.

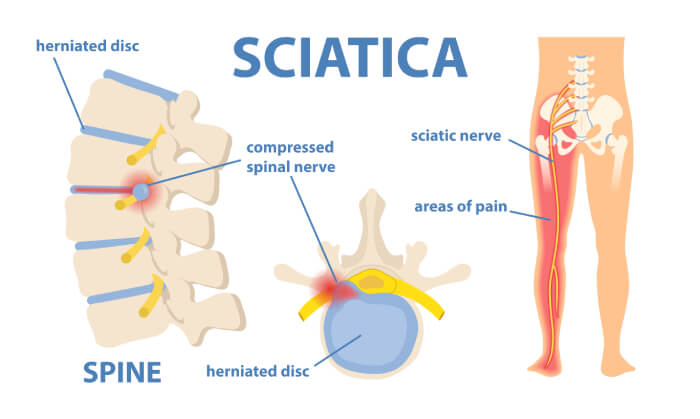
Sciatica
Sciatica occurs due to multiple reasons, one of them being Lumbar instability, Disc herniation or even SI Joint Instability.
SI Joint instability can present as sciatic pain in a number of ways. When ligaments are lax and loose, muscles around the joint tend to go into spasm, in order to try and stabilise the joint. This results in pressure on the nearby nerves, which run down the leg. Alternatively, excessive sacral motion may eventually directly aggravate the Sciatic nerve.
Another variation of sciatica is “Piriformis Syndrome,” which can occur alone or in conjunction with SI joint instability. If you consider the anatomy and see how close the SI joint is to the piriformis muscle, this is not difficult to understand.
If any of the pelvic ligaments are sprained, the resulting swelling will put pressure on nearby nerves that run down the leg. Just as a sprained ankle swells after an injury, so will sprained connective tissue in the pelvis, putting pressure on the sciatic (or other low back nerve roots) and causing “sciatica.”
The good news is that Prolotherapy can help. Let’s take a look at some case studies below:
CASE STUDY
Dextrose Prolotherapy for Unresolved Low Back Pain: A Retrospective Case Series Study
Hauser et.al (2009) treated one hundred and forty-five patients with Dextrose prolotherapy, who had been suffering from lower back pain for an average of four years and 10 months. The patients were administered therapy injections on a quarterly basis.
Fifty-five patients out of these were those who had been told that they had no other treatment option for their pain while twenty-six patients were told that surgery was their only option left.
Follow ups were taken about twelve months after the last Prolotherapy session. The patients were inquired about their pain levels, daily activity pre and post treatment and physical and psychological symptoms.
The results were accumulated and certain observations were made. The pain levels in these 145 patients decreased from 5.6 to 2.7 after Prolotherapy; 89% experienced more than 50% pain relief with Prolotherapy; more than 80% improved in walking and exercise ability, anxiety, depression, and overall disability; and 75% were able to stop taking pain medications completely. The pain reduction reached statistical significance, including the subset of patients told there were no other treatment options for their pain and those told surgery was their only treatment option.
It was deduced that patients with unresolved low back pain for more than four years were shown to improve their pain, stiffness, range of motion, and quality of life measures even 12 months after their last Prolotherapy session. This pilot study demonstrated that Prolotherapy is a treatment that should be considered and researched further for people who have unresolved low back pain.
Conclusion:
Prolotherapy is a revolutionary treatment for long-term chronic conditions and pain management. A safe, in-office procedure, treatment plans are built around 3 sessions over 2 months, based on the severity of the condition.
There has been increasing evidence that this simple procedure, which involves injecting with dextrose solution should be a part of clinical practice to help patients with chronic pain conditions.
So, take the first step towards a happy, pain-free life! Visit us! To book in for an examination or to discuss your prolotherapy options please visit our Booking Page or call us at 0333 772 9655.
Reference:
https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-021-04957-4
Hackett GS, Huang TC, Raferty A. Prolotherapy for headache; pain in the head and neck, and neuritis. Headache 1962; pp. 3-11.
Ross A. Hauser, Danielle Steilen, Ingrid Schaefer Sprague. Cervical Instability as a Cause of Barré-Liéou Syndrome and Definitive Treatment with Prolotherapy: A Case Series.European Journal of Preventive Medicine.Vol.3, No. 5, 2015, pp. 155-166. doi: 10.11648/j.ejpm.20150305.15
Ross A. Hauser, MD and Heather McCullough, MA. Dextrose Prolotherapy for headache and Migraine pain. Practical Pain Management. URL:https://www.prolotherapy.com/pdf-head-neck/HN-008-Dextrose-prolotherapy-for-headache-and-migrane-pain-(2012).pdf
https://www.ajmc.com/view/86-million-workdays-lost-annually-to-migraine-in-the-uk
M.M. Seven, O. Ersen, S. Akpancar, H. Ozkan, S. Turkkan, Y. Yıldız, K. Koca,
Effectiveness of prolotherapy in the treatment of chronic rotator cuff lesions,
Orthopaedics & Traumatology: Surgery & Research,
Volume 103, Issue 3,
2017,
Sabaah, H.M., Nassif, M.A. What is better for rotator cuff tendinopathy: dextrose prolotherapy, platelet-rich plasma, or corticosteroid injections? A randomised controlled study. Egypt Rheumatol Rehabil 47, 40 (2020). https://doi.org/10.1186/s43166-020-00040-3
Effectiveness of prolotherapy in the treatment of chronic rotator cuff lesions
Seven M.M., Ersen O., Akpancar S., Ozkan H., Turkkan S., Yildiz Y., Koca K.
(2017) Orthopaedics and Traumatology: Surgery and Research, 103 (3) , pp. 427-433.
https://www.prolotherapy.com/knee-conditions-for-prolotherapy.html
Grote W, Delucia R, Waxman R, Zgierska A, Wilson J, Rabago D. Repair of a complete anterior cruciate tear using prolotherapy: a case report. Int Musculoskelet Med. 2009 Dec 1;31(4):159-165. doi: 10.1179/175361409X12472218840924. PMID: 20802815; PMCID: PMC2929023.
Ada AM, Yavuz F. Treatment of a medial collateral ligament sprain using prolotherapy: a case study. Altern Ther Health Med. 2015 Jul-Aug;21(4):68-71. PMID: 26030118.
Radin E, Paul I, Rose R. Role of mechanical factors in pathogenesis of primary osteoarthritis. The Lancet. 1972 Mar 4; 299(7749): 519–522.
Driban JB, Hootman JM, Sitler MR, Harris KP, Cattano NM. Is Participation in Certain Sports Associated With Knee Osteoarthritis? A Systematic Review. J Athl Train. 2017 Jun 2;52(6):497-506. doi: 10.4085/1062-6050-50.2.08. Epub 2015 Jan 9. PMID: 25574790; PMCID: PMC5488840.
Rabago D, Patterson JJ, Mundt M, Kijowski R, Grettie J, Segal NA, Zgierska A. Dextrose prolotherapy for knee osteoarthritis: a randomised controlled trial. Ann Fam Med. 2013 May-Jun;11(3):229-37. doi: 10.1370/afm.1504. Erratum in: Ann Fam Med. 2013 Sep-Oct;11(5):480. PMID: 23690322; PMCID: PMC3659139.
Alderman D, 2007, Prolotherapy for knee pain, URL: https://www.prolotherapy.com/pdf-knee/KN-017-Prolotherapy-for-knee-pain-(2007).pdf
Ross A. Hauser, MD, Hilary J. Phillips, and Havil S. Maddela, 2010, Journal of Prolotherapy. 2010;2(3):416-437. URL: https://www.journalofprolotherapy.com/pdfs/issue_07/issue_07_05_meniscal_case.pdf
https://www.prolotherapy.com/knee-conditions-for-prolotherapy.html
https://www.prolotherapy.com/Tendinitis-and-tendinopathy-conditions-for-prolotherapy.html
Rabago D, Slattengren A, Zgierska A. Prolotherapy in primary care practice. Prim Care. 2010 Mar;37(1):65-80. doi: 10.1016/j.pop.2009.09.013. PMID: 20188998; PMCID: PMC2831229.
George J, Li SC, Jaafar Z, Hamid MSA. Comparative Effectiveness of Ultrasound-Guided Intratendinous Prolotherapy Injection with Conventional Treatment to Treat Focal Supraspinatus Tendinosis. Scientifica (Cairo). 2018 Jul 2;2018:4384159. doi: 10.1155/2018/4384159. PMID: 30057849; PMCID: PMC6051036.
Lokman Kehribar , Serkan Sürücü, European Journal of Public Health Studies – ISSN 2668-1056, Volume 1, Issue 1, 2021
https://www.prolotherapy.com/elbow-conditions-for-prolotherapy.html
Rabago D, Slattengren A, Zgierska A. Prolotherapy in primary care practice. Prim Care. 2010 Mar;37(1):65-80. doi: 10.1016/j.pop.2009.09.013. PMID: 20188998; PMCID: PMC2831229.
American Journal of Roentgenology. 2010;194: 1047-1053. 10.2214/AJR.09.3255
Read More: https://www.ajronline.org/doi/full/10.2214/AJR.09.3255
https://www.prolotherapy.com/foot-conditions-for-prolotherapy.html
Rabago D, Slattengren A, Zgierska A. Prolotherapy in primary care practice. Prim Care. 2010 Mar;37(1):65-80. doi: 10.1016/j.pop.2009.09.013. PMID: 20188998; PMCID: PMC2831229.
Ersen Ö, Koca K, Akpancar S, Seven MM, Akyıldız F, Yıldız Y, Özkan H. A randomised-controlled trial of prolotherapy injections in the treatment of plantar fasciitis. Turk J Phys Med Rehabil. 2017 Aug 12;64(1):59-65. doi: 10.5606/tftrd.2018.944. PMID: 31453490; PMCID: PMC6709612.
https://www.prolotherapy.com/lower-back-conditions-for-prolotherapy.html
Dextrose Prolotherapy for Unresolved Low Back Pain: A Retrospective Case Series Study. (2018, September 28). Journal of Prolotherapy. Retrieved September 27, 2022, from https://journalofprolotherapy.com/dextrose-prolotherapy-for-unresolved-low-back-pain-a-retrospective-case-series-study/#:%7E:text=In%20one%20study%20on%20chronic,evidence%20of%20the%20procedure’s%20effectiveness.
