Sciatica
For an assessment of Sciatica Contact us on 0333 772 9655 or book in on the ‘Book Now’ Tab above
What is Sciatica?
What is Sciatica and how does it present:
You go to the doctor concerned about a sharp pain that starts in the lower back and spreads down the buttock and thigh all the way down to the sole of the foot.
This is often accompanied by a burning pain or ‘pins and needles’ in the calf or foot. This is often how Sciatica first presents itself.
Sciatica affects approximately up to 5% of the population at sometime in their lives. Approximately 10% of these patients have symptoms that last longer than 3 months. The good news is that up to 80% of these patients make a recovery within 6 weeks.
In the days or weeks before presenting itself you may have been doing high impact activities or heavy physical work.
These activities may have been carried out with lots of bending forwards or repetitive twisting motion. The work doesn’t necessarily have to be heavy, it may just involve lots of low impact highly repetitive work.
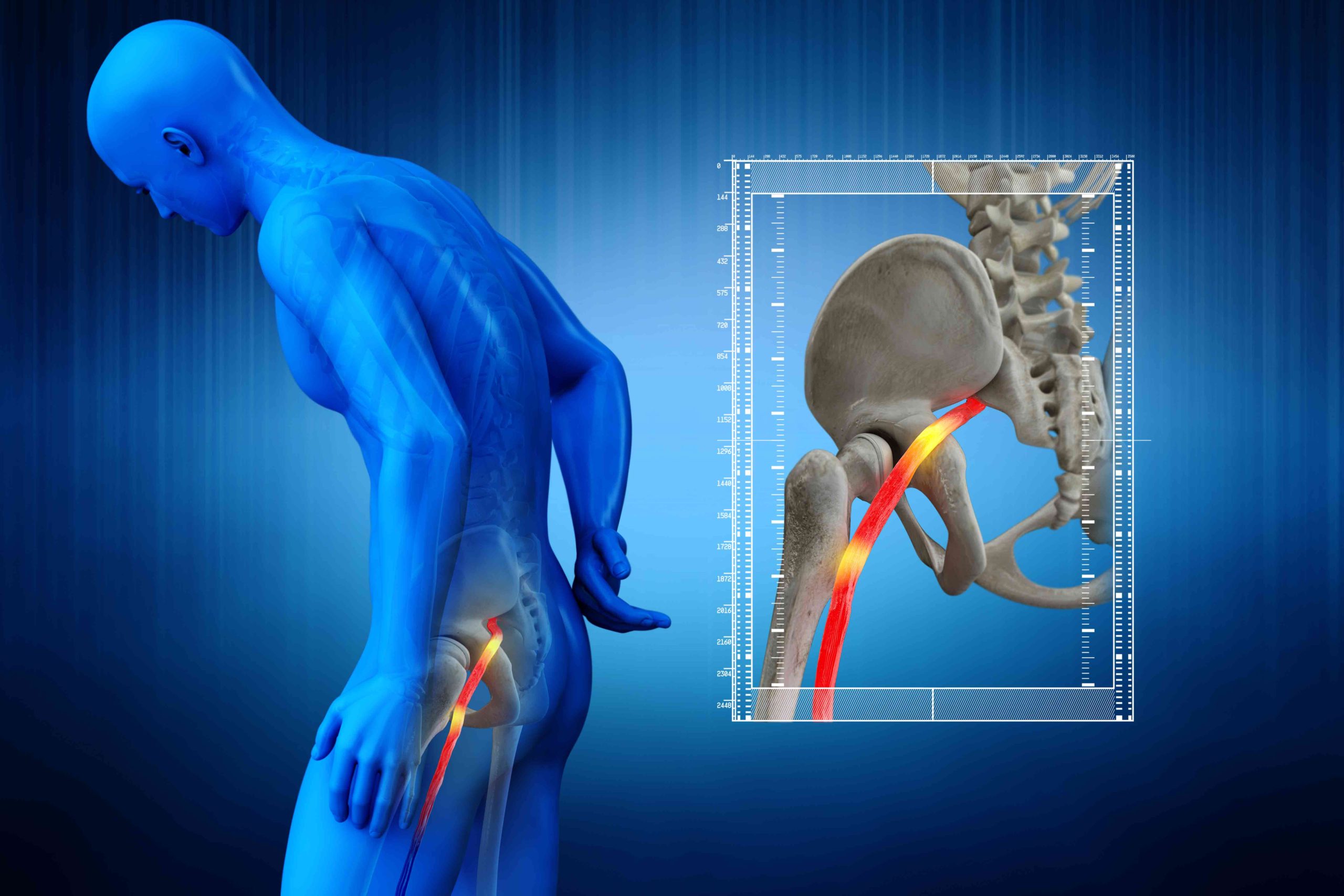
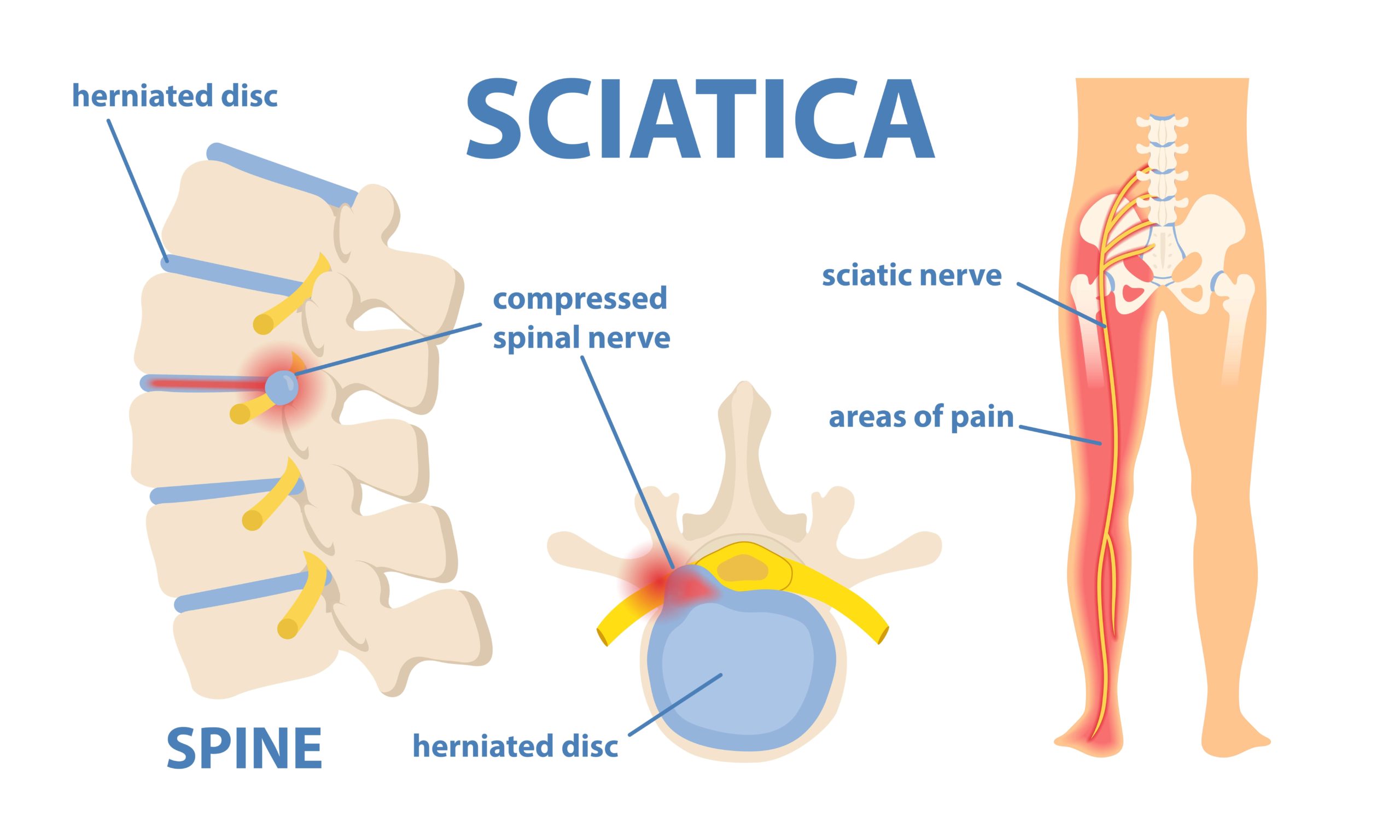
Sciatica refers to pain along the Sciatic nerve which runs from your lower back, buttock and all the way down the back of the knee to the foot and toe.
Often it will feel like a trapped nerve and you may experience ‘electric shock’ like pain spreading from the buttock to the sole of the foot or even big toe. Patients also describe it as a ‘deep throbbing pain‘ radiating down the leg.
Sometimes the pain may not spread all the way down the back of the leg and may stop at the back of the knee. True Sciatica however often spreads right down to the foot.
Patients also often complain of a very tight sensation in the buttock like a ‘muscular spasm’ which feels better after soft tissue therapy.
It is one of the most common causes of lower back pain. It commonly affects patients in their late 30’s or 40’s.
Sciatica itself has a relapsing – remitting course meaning you may often find yourself as pain-free between bouts and then a few weeks or months are spent in agony dealing with the pain when it returns.
The Sciatic nerve is the nerve in red highlighted in the picture below. It is the longest and largest nerve in your body.
What causes Sciatica?
The most common cause of Sciatica is compression and inflammation of the Sciatic Nerve itself.
What causes this to happen? Often a Disc Bulge or a condition called Spinal Stenosis.
The terms Disc Herniation, Disc Prolapse or Slipped Disc are often used to describe the same problem.
You may actually recall the exact moment Sciatica occurs following lifting an object, cleaning, gardening or exercising. It may even occur without any noticeable trauma in a gradual manner.
Contrary to popular opinion, Sciatica does not always occur after heavy lifting. It could be related to repetitive low impact movements where certain repeated movements of the spine cause repeated stress on the spinal discs over time.
All it then takes is for a simple bending or twisting movement of the spine when it is vulnerable to lead to disc rupture or prolapse with release of contents or pressure onto the Sciatic Nerve. Severe pain which increases in intensity then follows over the coming days and weeks.
Why is Sciatica so painful?
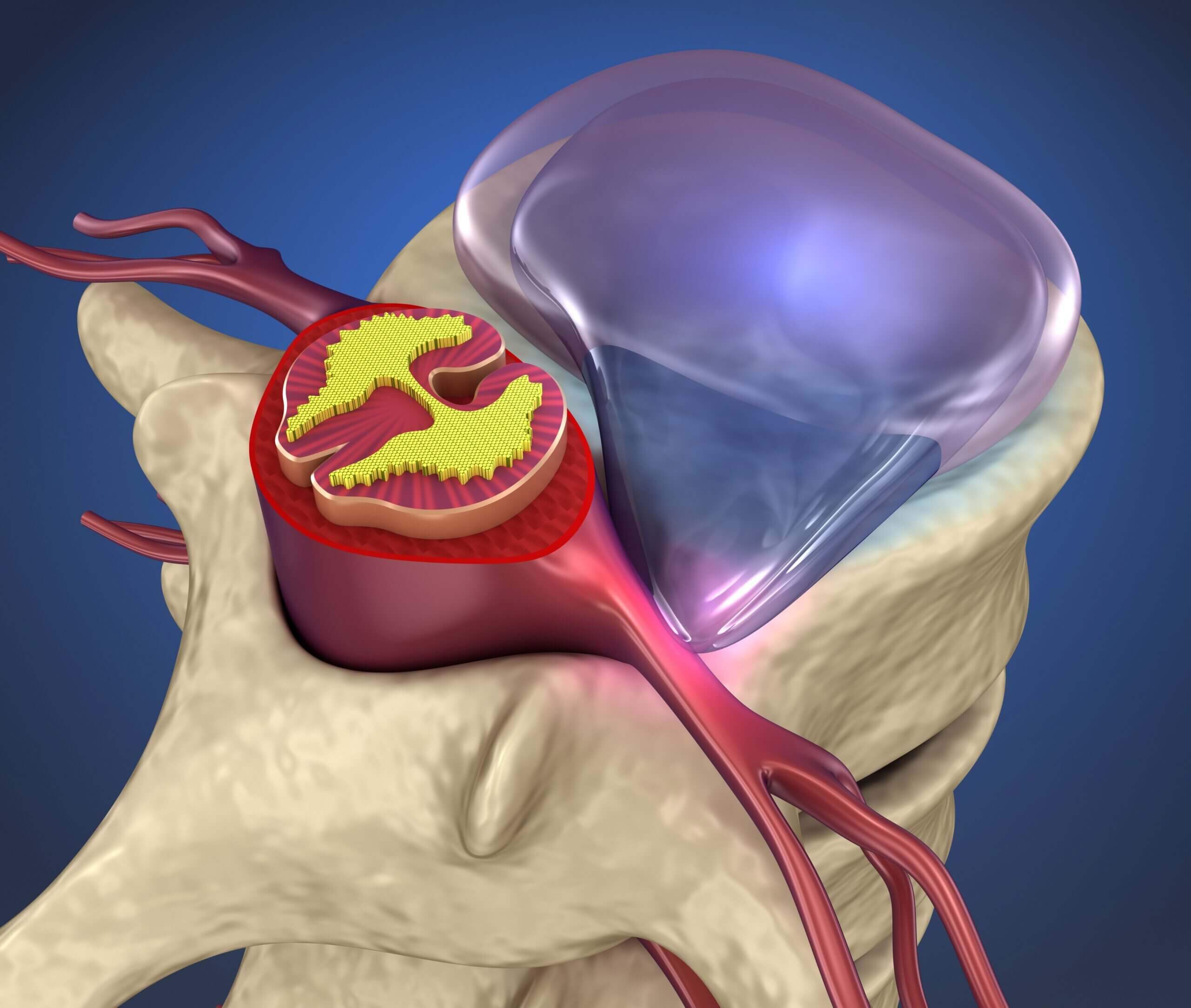
When the Sciatic Nerve is compressed by a Disc Herniation or the bony aspect of the spine (due to an osteophyte or a mass), the Sciatic Nerve itself becomes swollen which increases the pressure inside it.
This can lead to ‘burning‘ or ‘electric shock‘ like pain within the nerve.
Another reason why Sciatica may be painful is that when the disc is injured, the leakage of disc material (the central material of the disc called Nucleus Pulposus) onto the Sciatic Nerve may cause an Inflammatory reaction within the nerve.
This may damage the nerve and cause pain. The pain you experience going down the leg is often due to this. This is often referred to as ‘radicular pain’.
Pain doesn’t always accompany Sciatica. Sometimes it may just be ‘pins and needles’ or ‘numbness’ in the back of the thigh/calf or big toe.

Why is it that you don’t always get back pain in Sciatica?
Because Disc bulges occur in different directions. Often the direction the Disc herniation occurs in can dictate the symptoms experienced.
When a clinician performs the Slump test or the Straight leg raise test (Lasegue Test) on a patient, the pain of Sciatica is often reproduced. This is why these tests are often performed if Sciatica or lumbar disc herniation is suspected.
Why are the slump test and straight leg raise tests effective in detecting Sciatica?
In these tests the Sciatic Nerve is being stretched over the lumbar disc prolapse causing the Sciatica symptoms to be reproduced.
The Straight Leg Raise Test is shown in the youtube video below.
The Slump test and Straight leg raise test are two excellent diagnostic tests for Sciatica.
They are performed as part of an overall clinical history and examination.
In addition to these tests. the power, reflexes and sensation of the legs are also checked.
The Nerves and Muscles examined often correspond to L2, L3, L4, L5, S1-S4 in a thorough lower limb clinical examination.
An important question to ask is also whether the patient has experienced any urinary symptoms (weak urinary stream or incontinence (urinary/faecal) and any numbness in the back passage area.
Why is this? Read the ‘When is Sciatica serious‘ section below
Other Causes of Sciatica

Arthritis
Often especially after the age of 60, small bony spurs called Osteophytes can irritate the Sciatic nerve as it exits the lumbar spine

Spinal Stenosis
This is where a narrowing of the Spine in the intervertebral foramen where the Sciatic nerve exits may cause pressure on the Sciatic Nerve

Spondylolisthesis
A forward slippage of the spine which may be present from a young age may cause pressure/tension on the Sciatic Nerve. Often in this situation you get the symptoms in both legs. Certain rehab exercises must not be performed if this is the cause.

Back Injury
Occasionally a sudden trauma to the back e.g. a car accident, accident at work or sporting injury can also cause Sciatica.

Degenerative Disc Disease
A gradual ‘wear and tear’ of the discs which act as shock absorbers between the vertebrae.

Occupation
Especially if it involves heavy lifting, twisting your back or prolonged driving. Sedentary desk jobs can also lead to Sciatica

High BMI
Being overweight is a risk factor for Sciatica due to the additional stressors placed on your spinea

Pregnancy
Many patients also get a flare up Sciatica in pregnancy. This is often but down to the additional weight causing strain on the back
Clinical Symptoms of Sciatica
- What starts as low back pain may be followed by pain ‘shooting down the leg’. This may be felt like a sharp pain in the buttock or back of the thigh which spreads down to the ankle or foot. In some cases the pain can spread to the toe.
- Some times this pain is confused as hip pain and the patient complains of ‘pain in the hip’ or on the ‘outer’ aspect of the hip spreading down the leg. The hip regions does include the pathway of some of the nerves involved in Sciatica therefore Sciatica is sometimes mistakenly believed to be hip pain. A thorough clinical examination of the hip joint can often tell the clinician wether it is Sciatica or a hip problem.
- What about the pain of Sciatica itself? It is often severe and made worse by bending forward, coughing, sneezing, getting in and out of the car or doing simple things like depressing the clutch when driving.
- Patients will often struggle to adopt a comfortable seating position and sleep is often interrupted
Tests and Investigations for Sciatica
If symptoms are persisting for more than 6 weeks then ideally an MRI should be ordered to confirm the diagnosis.
MRI will often show the prolapsed disc and should be performed where there is a neurological deficit on examination (loss of sensation, power or muscle bulk in the legs or numbness in the back passage area).
A more urgent MRI may be required if features of Cauda Equina are present (see below)
Is a back xray useful in Sciatica? The answer is not as simple as a Yes/No.
Often an xray only shows the bone elements so disc prolapse. Hence, soft issue can rarely be imaged on an xray.
However an xray if analysed carefully by an experienced clinician can show osteophytes or spondylolisthesis or reduced disc spaces which could indirectly point towards the cause of Sciatica.
It may also show serious pathology such as a potential tumour so it is still a useful investigation if MRI is not accessible
To examine a potential disc prolapse however an MRI is preferred.
Lets have a look at what a disc prolapse looks like on an MRI scan.
Below is a cross section of an MRI scan sideways through the lower back (lumbar region). This is termed the Sagittal view.

The best and perhaps rather crudest way to describe the sagittal view is taking a saw and cutting a person in half from head down sideways on!
If we look carefully at the image we can see white coloured discs that have a small oval shape that run down the column in a stepladder fashion.
As we go down the column we can see a disc that is darker than the others and has a small dark circle protruding from it on the right side. (the red line indicates this disc in the picture)
This is actually what a disc prolapse looks like. This prolapse then compresses/irritates the Sciatic nerve which exits the spine. The resulting pain is termed Sciatica
Occasionally EMG studies may be performed if the MRI scan is normal to see if the Sciatic Nerve is involved. If the MRI appears normal and clinically there is still a sign of a prolapsed disc there is also the option of an upright MRI.
This is an MRI performed with a patient sat upright in different positions to see if the disc prolapse only occurs in some positions. Most of the time we do not have to resort to this but it is an option in rare cases
Treatment for Sciatica
- Depending on the profession, the treatment approach will vary although there is an overlap in terms of treatment techniques between manual therapists: Physios, Osteopaths and Chiropractors.
- A Doctor may prescribe you anti-inflammatory medication Ibuprofen/Naproxen and Amitryptiline/Gabapentin. Amitryptiline is an older anti depressant but in low doses for a short duration it is safe to use as a nerve painkiller. The only major pitfall is its ‘sedative effect’ on daily tasks.
- At MyMSK Clinic we use a combined approach of spinal injections and osteopathy as well as giving rehab exercises to hep you manage this debilitating condition.
Which specialist should i see for treatment of Sciatica?
Physiotherapist
A Physiotherapist may show you several postural refinements and exercises to help alleviate the pain. Mobilisation exercises such as ‘Nerve gliding‘ or ‘Nerve flossing‘ may be shown alongside the Mckenzie method of rehabilitation.
Osteopath
An Osteopath may follow a similar approach. Osteopaths generally deal with a greater proportion of back pain than other muscular issues and may attempt to perform a combination of manipulation and soft tissue therapy techniques.
Chiropractor
A Chiropractor will also take a similar approach to an Osteopath and attempt ‘Spinal Manipulations’ and ‘Positional Release’ of certain muscles around the Sciatic Nerve to help ‘release’ the Sciatic nerve

Why should i not get my back cracked in Sciatica?
Biomechanically if a torque force is applied to a damaged disc then this may lead to further pressure to the disc and damage to its internal components with a potential leakage of disc contents (gel like material called the Nucleus Pulposus) making the pain worse than it was originally!
A gentle manipulation in the thoracic area (upper back) may however release muscle spasm further up the spine and take away some of the stress on the lumbar discs.
Many physical therapy approaches have their place in the treatment of Sciatica. The more advanced practitioner is able to select the best treatment based on the onset/recurrence/age and other additional symptoms
In the majority of cases Sciatica does settle with Painkillers, Rest and Physical therapy approaches (depending on your chosen approach) and activity/posture modification
We at MyMSK Clinic strongly advise that one size does not fit all in terms of treatment or rehabilitation exercises.
Certain movements you may think are safe in disciplines like yoga/pilates can actually make Sciatica worse due to the extreme ranges of motion the spine adopts in certain movements. These extreme ranges can cause uneven pressure on the disc and cause pain to recur if you already suffer from Sciatica
When in severe pain physiotherapy exercises can be very difficult to perform. In this instance spine injections can help greatly to break the pain cycle and allow you to resume physical therapy
When is Sciatica serious?
If we feel it is a serious case of Sciatica with a large disc herniation which may press on the spinal cord causing irreversible nerve damage, we will arrange an urgent private MRI scan at one of our associated scanning facilities
If you are over the age of 55 and have a new case of Sciatica with weightloss and night sweats it is important to see a doctor urgently as you may need an urgent examination and blood tests.
If you find that one leg is weaker than the other or you are dragging one foot behind you, it is important to consult a doctor urgently to get an MRI scan as you may have a large disc herniation which may cause irreversible nerve damage.

Sciatica Treatment

Spinal Injections
We offer a range of spinal injections that may include Caudal Epidurals, Trigger Point injections, Facet Joint Injections, Sacroiliac Joint injections and Prolotherapy in the Spine.
Explore More
Cortisone Injections
A Cortisone Injection (termed steroid injection in the UK) is an anti inflammatory injection for the joints or body tissue to relieve pain.
Explore More
Platelet Rich Plasma
PRP treatment can reduce the need for anti-inflammatory medication or strong painkillers with unwanted side effects
Explore More
Prolotherapy
A regenerative treatment for chronic painful joints and ligaments which involves the injection of a specially formulated solution into damaged tissue.
Explore MoreFor an Assessment of Sciatica
Book in at MyMSK Clinic with our online Booking Page or call us on 0333 772 9655
Contact us
We’d love to hear from you!
Just reach out and contact us via any of
these channels:

Call us on

Email us on

Call us on

