
Dead leg or its alternative name ‘Quadricep Contusion’ is a traumatic blow to the upper leg commonly seen in Football, Rugby, MMA and other high-impact ‘contact’ sports.
As the name indicates, a dead leg refers to the loss of sensation in the lower limbs. The numb feeling can occur in a single limb or both limbs (unilateral or bilateral) and extend to your toes.
When the body receives a direct blow, the quadriceps muscles are crushed against the femur (thigh bone). As a result, the muscle fibres and small blood vessels in the impact area are damaged. This results in a swelling full of blood within the thigh muscles (known as quadricep muscles)

Numbness in the thigh generally occurs due to nerve entrapment. This is due to the increased pressure within the thigh muscles from the swelling which then compress the nerves.
Quadriceps muscles are a group of four muscles located in the front of your thigh. They facilitate many movements, such as walking or running. In addition, they also help flex the hip and straighten the knee.
A Quadricep contusion can be quite painful, particularly in the first few hours of impact, followed by tingling and numbness of the leg. This happens when the thigh muscles start to stiffen up after the injury.
Symptoms of Dead Leg
The primary symptom of a dead leg is the pain at the point of impact. In minor cases, you can even continue playing; however, the pain may increase once the muscle cools down, followed by gradual tightening and stiffening of the quadriceps muscles.
As with every injury, dead legs can have three degrees of severity. Of these, grade 1 or milder contusions are more common.
Grade 1 – Mild Contusion
In a grade 1 thigh contusion, there’s a tightness to the thigh, with the injury site being sore to touch. However, there may not be swelling, and you will have a full range of motion although you may experience difficulty walking without a limp

-
- Difficulty walking without a limp
-
- Minimal or no swelling
-
- Minimal or no loss in the range of motion
-
- Mild pain with thigh contraction
Grade 2 – Moderate Contusion
As with grade 1 contusion, you will experience pain on the injury site with a prominent swelling. Furthermore, you will walk with a pronounced limp as weight-bearing will bring on more pain.
-
- Walking with a limp
-
- Moderate swelling
-
- Sharp pain or muscle tension during movements
-
- Bruising
-
- Pain with thigh contraction
-
- Restricted movements in the knee
Grade 3 – Severe Contusion
With grade 3 contusions, you cannot walk without a walking aid such as crutches. Severe pain and significant swelling are also indicative of extensive damage.
-
- Unable to walk without a walking aid
-
- Acute pain throughout the thigh
-
- Extensive swelling and bruising
-
- Muscle deformity
-
- Reduced range of motion in the knee
Causes of Dead Leg
Dead leg or quadricep contusion happens when you receive a hard, direct hit to your thigh. The force of impact causes the muscle to tear and bleed, but the sheath remains intact. Often, an undamaged sheath is more painful and is considered more serious. This is because the blood cannot flow out, causing an increase in pressure as the compartment expands.
In more severe cases, it can tear the sheath that covers the muscles, which causes internal bleeding. However, the blood flows and spreads out. As a result, there’s no heightened pressure, resulting in less pain and movement restriction. Nevertheless, there can be discolouration and bruising.
Most episodes of dead leg occur during sports especially contact sports or high impact sports such as football or lacrosse:
-
- From the knee of an opponent colliding with the quadricep muscles during a tackle or running
-
- From equipment such as a ball in cricket or getting hit with a stick in hockey
In addition, it can also happen in sports such as snowboarding, skateboarding or skiing when someone falls over or hits their thigh on a hard surface.
Diagnosis of a Dead Leg
Generally, there’s no standardised testing to diagnose a dead leg. Instead, the doctor diagnoses a dead leg by inquiring about the injury and the symptoms. The range of motion after the first 24 hours indicates the extent of the damage. The more the movement, the less the damage.

With rest and treatment, your dead leg should heal on its own within the prescribed timeline. If not, the doctor may suggest an urgent MRI scan to look at the injury.
Complications of Dead Leg
A Dead leg can be treated with minimal side effects and complications. However, there can be complications without appropriate treatment, namely Myositis Ossificans and Compartment Syndrome.
Myositis Ossificans
This is a condition where bone tissue forms within the muscle. The symptoms include:
-
- A lump at the injury site
-
- Severe pain accompanied by swelling and bruising
-
- Severe pain during muscle activation
-
- A significant reduction in the range of motion in the knee
Myositis Ossificans is a long-term complication of a dead leg/Quadriceps Contusion. Depending on the severity, it can become debilitating and requires early intervention. If the lump compromises blood circulation or nerve conduction, your doctor may prescribe surgery. If so, the recovery time can take as much as 12 months.
How does Myositis Ossificans occur?
Often immediately after trauma, a blood swelling forms within the muscle (due to a muscle tear). In this case it often will need to be aspirated or drained or allowed to slowly move into surrounding tissues and disappear. However, tissue massage over the area during this time may lead to ‘ossification’ of the fluid area.
Compartment Syndrome
Compartment syndrome can occur when the pressure within the muscle compartments increases. This may cause pinching of the major arteries and nerves within the leg. This may cause areas of the tissue to die if not drained in time. Compartment Syndrome is a medical emergency.
The most common symptom associated with compartment syndrome is intense pain in the upper leg area. You may also experience other symptoms such as:
-
- Swelling or inflammation
-
- Restricted range of motion
-
- Pins and needles & Numbness
-
- Stiffness
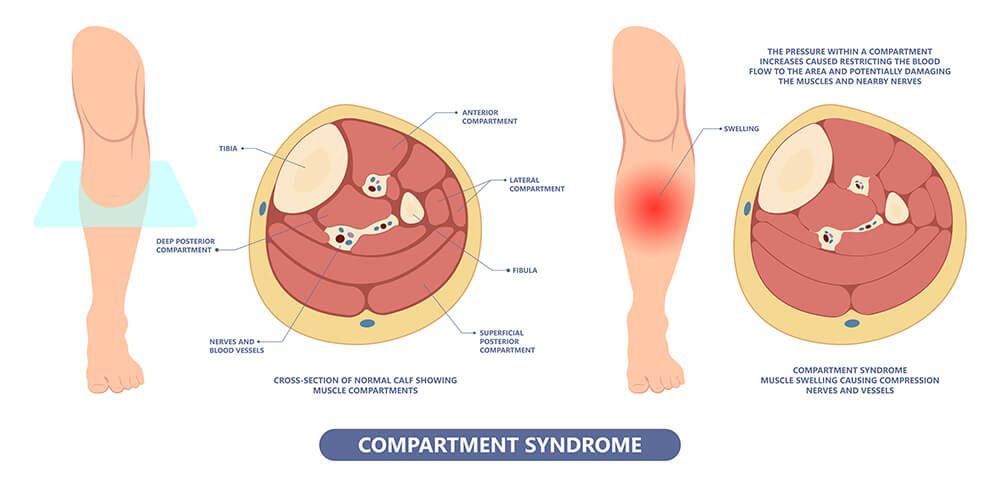
The 5 ‘P’s are often associated with Compartment Syndrome. Pain, Pallor (Pale skin tone), Paresthesia (numbness), Pulselessness (faint pulse) and Paralysis (weakness with movements)
Consult with a doctor immediately if you have any of the symptoms above by attending the nearest A&E.
You may have various tests, including X-rays and an MRI. Severe Compartment Syndrome may also require surgery to relieve the building pressure within the compartments.
Treatment of Dead Leg
The first 24-48 hours are crucial for a Dead leg. First, follow the RICE regime to limit the damage and speed up the recovery process as soon as the injury occurs. RICE stands for Rest, Ice, Compression and Elevation. This decreases the blood flow to the region, reducing swelling in the injured area. In addition, the RICE regime helps reduce tissue damage.
-
- Rest: Limit the amount of weight you put on your injured leg. Use crutches or any other walking aid if you have trouble walking.
-
- Ice: Apply ice to the dead leg for 15-20 minutes every 1-2 hours. A bag of peas or ice wrapped in a damp cloth would do.
-
- Compression: Apply an elastic bandage over the injured area. Ensure that it is firm but not tight.
-
- Elevation: Lay down with your leg elevated on a chair or pillows. This is to ensure that it is above the level of your heart.
Continue with the RICE principle until you see a Clinician. .
To start with, the aim of treatment is to bring down the pain and swelling. During this time if there is a hematoma detected on ultrasound imaging, this may be aspirated. After this, the treatment plan may include gentle mobilisation and rehab exercises.
Final Thoughts
While you cannot prevent a dead leg, especially for athletes, you can follow the prescribed treatment process to ensure a complete recovery. However, since muscle damage is expected in a dead leg, the recovery process is gradual. Therefore, it is critical that you do not return to your sport soon, particularly for those with grade 2 and grade 3 contusions.
It is also crucial that you consult with a doctor and get assessed to rule out any possible damage to the bone. If your symptoms worsen (increase in pain or swelling), seek immediate medical attention.
Here at the My MSK Clinic, we are happy to assess your leg injury if you suspect a Dead Leg and help you recover faster.
Frequently Asked Questions
- Is a dead leg serious?
A dead leg is usually not serious as long as you undergo appropriate treatment and take enough rest. If not, it may lead to complications such as Myositis Ossificans and Compartment Syndrome.
- How long can a dead leg last?
A dead leg can last from a couple of weeks to months depending on the severity of the injury. However, you should not return to play until you reach the full range of motion and achieve full strength.
- What is the recovery time for a dead leg?
The recovery time for a dead leg depends on the severity of the injury.
-
- For a Grade 1, you should be able to return to play in 2-3 weeks.
-
- For a Grade 2, the recovery time is 4-6 weeks. The longer duration is due to the increased damage to the muscles.
-
- For a Grade 3, the recovery time is eight weeks. This can increase depending on the extent of the injury.
- How to prevent a dead leg?
While you cannot prevent a direct impact, especially in sports, you can follow the below steps to reduce your chances of injury.
-
- Wear well-fitting supportive or protective equipment such as padding over the thigh (i.e especially in sports such as Cricket and Lacrosse).
-
- Ensure that you are hydrated and take enough water.
-
- Strength and conditioning exercises to make sure the quadricep muscles are strong
-
- Warm-up and cool-down routines.




