Piriformis Syndrome
Introduction to Piriformis Syndrome
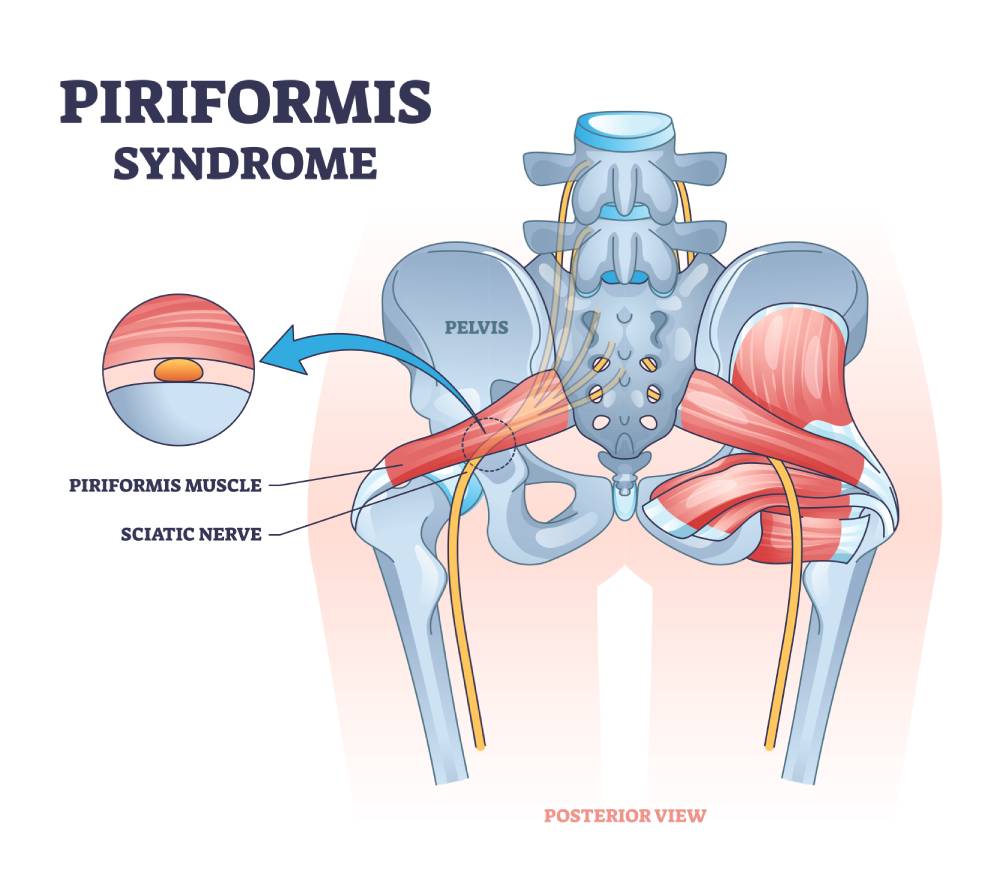
Piriformis Syndrome is an injury or irritation of the piriformis muscle situated in the buttock region. This condition can lead to cramping and persistent pain in the buttock area.
If left untreated, the affected piriformis muscle may also exert pressure on the nearby sciatic nerve, leading to nerve irritation and causing Sciatica.
Individuals experiencing this syndrome often report discomfort, numbness, and tingling in the buttock, radiating down the back of the thigh down to the foot.
Understanding the symptoms of Piriformis Syndrome and early intervention is crucial in managing this condition effectively.
In this article, we delve a little deeper into this syndrome.
Piriformis Anatomy
A pear-shaped muscle, the Piriformis muscle is present in the gluteal (hip) region
One of the major nerves of the lower spine and limb, the sciatic nerve, passes under it.
In a small proportion of patients, the Sciatic nerve may pass through the piriformis muscle or even above it.
It also lies beneath the gluteus maximus muscle.
Its role is to rotate the leg outward when the hip is flexed during walking which is important to help the balance and gait (Chang et al., 2022).
When the thigh is raised during hip flexion, the Piriformis muscle becomes an internal rotator of the hip.
These movements are essential in turning your leg and foot outward as you walk, allowing for a smooth transfer of body weight to the other side.
The Piriformis muscle contributes to the fluidity and stability of your gait as you move through each step of your journey.
How Does Piriformis Syndrome Present?
Patients may experience Sciatica like symptoms.
Common symptoms include:
-
- Burning or shooting pain down the back or outside of the hip and leg
-
- Numbness and/or tingling in the buttocks
-
- Dull ache or pain in the hip region
-
- Pain aggravated on sitting
-
- Loss of power in the lower legs causing a limp
How does one Sit with Piriformis Syndrome?

Piriformis syndrome can worsen due to prolonged sitting and may eventually lead to the person being unable to sit for lengthened periods of time.
Learning how to sit with Piriformis Syndrome is essential in managing its symptoms, and certain things need to be considered, which include:
-
- Posture – while sitting, keep shoulders back, feet resting on the ground, avoid raising your knees higher than the level of the hips. Sitting cross-legged can also aggravate the condition (Snijders et al., 2005)
-
- Support – adding seat cushions, lumbar support, and a footrest if needed, can help take the pressure off the Piriformis muscle or Sciatic Nerve, easing the pain. Ergonomic chairs and desks are specifically designed for this purpose
-
- Breaks – if sitting is required for longer periods, make sure to take adequate breaks from time to time, and get up and stretch for a bit
How to Sleep with Piriformis Syndrome?
In this condition, sleeping can either be difficult because of the pain, or the pain can be affected by sleep posture.
There are a few ways to try and minimize the chances of this happening.
Some things can be incorporated into your sleeping routine to ease the symptoms:
-
- Support – Use mattresses and pillows that provide the best support to your back
-
- Sleep positions – Sleeping on your back, add two pillows under the knees to slightly raise them, and while on the side, place a pillow between your knees. This keeps the muscle relaxed while you sleep.
-
- Stretch – body stretches before sleeping can help relax the tense piriformis muscle, leading to increase in quality of sleep. The stretch we recommend is lying on your front and stretching outwards with the arms and legs for 30-60 seconds
-
- Heat pad/patch on the muscle at night can also work (practice care when doing this)
What if my Piriformis Syndrome Won’t Go Away?
If Piriformis Syndrome is not managed properly, it can become a chronic condition.
In mild cases, the person suffering from this issue is usually given some over-the-counter painkillers, including NSAIDs like ibuprofen or naproxen.
However, if the pain is not relieved, stronger analgesics, like opioids or muscle relaxants or neuropathic painkillers, may need to be prescribed.
Physical therapy including deep tissue massage, dry needling, and manipulation techniques can be useful in cases where routine activities, such as sitting, or walking are affected.
The range of motion improves significantly, leading to pain relief and better mobility overall (Tonley et al., 2010).
Heat therapy can also prove beneficial if Piriformis syndrome won’t go away, as it loosens tight muscles and helps relieving nerve compression.
On the other hand, icing can reduce any swelling in the region, promoting healing of the muscle and nerve.
In case of chronic and recurrent pain that significantly affects activity, a painkilling injection into the region containing an anti-inflammatory medicine may be administered, which reduces the symptoms and improves the quality of life (Vij et al., 2021).
When all treatment options have failed, an MRI of the lower lumbar or pelvic region may be required to try and see the structure of the muscle and its relation to the nerve
This is to check any co-existent disc pathology and to assess the sacroiliac region to exclude an SI joint issue.
Often with injections and rehab, most cases of Piriformis syndrome do resolve and surgery is advised as a last resort.
Is Walking Good for Piriformis Syndrome?
In this condition, walking can prove to be quite a painful activity, and a lot of patients might start avoiding it altogether.
However, lack of physical activity can be even more harmful, as the muscles weaken, and the overall power of the midsection and lower legs declines.
To help, the patient needs to make some modifications during walking.
-
- If walking helps with pain – take a few short walks in the week
-
- If walking increases pain, then stop and get evaluated by a Doctor.
-
- Walking with upright posture is important, walk with your back straight, tuck in your stomach, keep your shoulders back
-
- Focus on breathing evenly throughout
Piriformis Syndrome V Sciatica
The close connection between the piriformis muscle and the sciatic nerve is relevant to lower body movement. This muscle extends on both sides of the body, contributing to nearly every lower body movement, while the sciatic nerve courses beneath the muscle.
As the body’s largest nerve, the sciatic nerve originates from the spinal cord, travels under the buttock muscle (Gluteus Maximus), and extends down the back of the legs, reaching the feet.
While this syndrome and sciatic pain share certain common features in their symptoms, it is crucial to distinguish between the two as they represent distinct conditions.
This syndrome often goes misdiagnosed or underrecognized, primarily due to its resemblance to sciatica nerve pain.
Differentiating these conditions is vital to ensure accurate diagnosis and effective treatment, preventing potential mismanagement.
Test for Piriformis V Sciatica
Piriformis syndrome is a condition which may cause Sciatica due to the structure and anatomy of the Sciatic nerve.
So how do we tell if its Piriformis syndrome or Sciatica?
The straight leg raise test (Lasegue’s Maneuver) is performed as a general test for Sciatica, but to differentiate between the two, a special test is required.
This can then lead to correct treatment and earlier recovery.
The FAIR test (stretching the muscle by Flexion, Adduction, and Internal Rotation) is performed by having the patient lie on their side, and passively flexing, internally rotating and adducting the hip. The test is positive for piriformis syndrome if this test causes pain. (Chen & Nizar, 2012).
Causes and Risk Factors of Piriformis Syndrome
Anyone can suffer from Piriformis Syndrome, but the individuals who are at risk include:
-
Females, as this syndrome is most likely to develop in females, and the female to male ratio is 6:1.
-
Anatomic variations in the positioning and location of the sciatic nerve (occasionally the Sciatic nerve can travel through the Piriformis muscle
-
Any direct damage or injury to the hips or buttocks.
-
Sitting for long hours.
-
Repetitive physical movements like long-distance running, cycling or walking.
Diagnosing Piriformis Syndrome in Runners
This syndrome in runners is frequently identified by assessing distinctive symptoms, including tenderness and inflammation of the gluteal muscles, sharp pain in the centre of the buttocks, and discomfort experienced during walking or running.
A comprehensive physical examination should be conducted, and when necessary, additional investigative steps are often taken, such as ordering X-ray or MRI scans to exclude other pathology and assess the piriformis muscle.
Clinicians can accurately diagnose Piriformis Syndrome through this meticulous approach, enabling them to tailor an effective treatment plan that facilitates the runners’ recovery and ensures their swift return to the track.
-
Imaging and Other Diagnostic Tests
Different diagnostic tests can be performed to identify Piriformis Syndrome, such as X-ray, MRI, Ultrasound or Nerve Conduction Studies (to exclude a Sciatic nerve issue).
Clinicians can also carry out some Physical Tests around the hip to see how your body reacts to stretching or activating your Piriformis muscles.
Runner’s Piriformis Syndrome
Piriformis syndrome is more common in athletes who run. The muscle rotates the hip, helps to balance weight on one leg, and engages actively during running along with other stabilizers of the hip joint to keep the pelvis in place, every time the foot hits the ground.
In runner’s piriformis syndrome, the muscle is at a greater risk of spasm because of fatigue and overuse. If the symptoms interfere with running, a few changes can be made to prevent their worsening, and long-lasting damage, like:
-
- Avoid running everyday for long periods or reduce running load
-
- Running uphill should be stopped while pain is present
-
- Alternate between heavy and light training weeks
-
- Ensure that you get adequate amounts of rest
Conclusion
Piriformis syndrome can significantly affect a person’s life, making simple activities like walking and sitting quite painful. However, consulting a doctor when your symptoms start to show, can prevent the condition from worsening, and aid in quicker recovery.
References
- Chang, C., Jeno, S.H. and Varacallo, M. (2022) Anatomy, Bony Pelvis and Lower Limb, Piriformis Muscle, National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/books/NBK519497/
- Roy, B.A. (2014) Piriformis syndrome : ACSM’s Health & Fitness Journal, ACSM’s Health And Fitness Journal. American College of Sports Medicine. Available at: https://journals.lww.com/acsm-healthfitness/fulltext/2014/07000/piriformis_syndrome.
- Snijders, C.J, Hermansa, P.F.G. and Kleinrensink, G.J. (2005) Functional aspects of cross-legged sitting with special attention to piriformis muscles and sacroiliac joints, Science Direct. Clinical Biomechanics. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0268003305002135
- Steiner, C. et al. (1987) Piriformis syndrome: Pathogenesis, diagnosis, and treatment, De Gruyter. De Gruyter. Available at: https://www.degruyter.com/document/doi/10.1515/jom-1987-870422/html
- Tonley, J.C. et al. (2010) Treatment of an individual with piriformis syndrome focusing on hip, JOSPT. Journal of Orthopaedic and Sports Physical Therapy. Available at: https://www.jospt.org/doi/full/10.2519/jospt.2010.3108
- Vij, N. et al. (2021) Surgical and non-surgical treatment options for piriformis syndrome: A literature review, Anesthesiology and pain medicine. U.S. National Library of Medicine. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8241586/#:~:text=and%20functional%20ability.-,Physical%20therapy%2C%20steroid%20injections%2C%20botulinum%20toxin%20injections%2C%20and%20dry,are%20available%20if%20treatment%20fails
- Mondal, M. et al. (2017) International Journal of Health Sciences and Research, Research Gate. Available at: https://www.researchgate.net/profile/Pravin-Kumar-29/publication/318318389_Prevalence_of_Piriformis_Tightness_in_Healthy_Sedentary_Individuals_A_Cross-Sectional_Study/links/596376b90f7e9b819490651b/Prevalence-of-Piriformis-Tightness-in-Healthy-Sedentary-Individuals-A-Cross-Sectional-Study.pdf
- Chen, C.K. and Nizar, A.J. (2012) Prevalence of Piriformis Syndrome in Chronic Low Back Pain Patients. A Clinical Diagnosis with Modified FAIR Test, Wiley Online Library. Pain Practice. Available at: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1533-2500.2012.00585.x