Overview of Osteoarthritis and Its Impact on Quality of Life
Osteoarthritis (OA) is the most common form of arthritis in the UK, arising when protective cartilage cushioning our joints gradually wears away.
As the cartilage thins and deteriorates, patients experience increasing pain, stiffness and reduced mobility.
Everyday tasks—climbing stairs, carrying shopping or simply walking—can become arduous, often leading to disrupted sleep, low mood and withdrawal from social activities.
Over time, the combination of physical discomfort and emotional strain can significantly diminish overall quality of life.
Emerging Role of Injectable Therapies in Joint Preservation
While weight management, physiotherapy and oral pain relief remain the cornerstones of OA treatment, their benefits are frequently modest or short‑lived.
Injectable therapies have therefore emerged as a valuable, minimally invasive option.
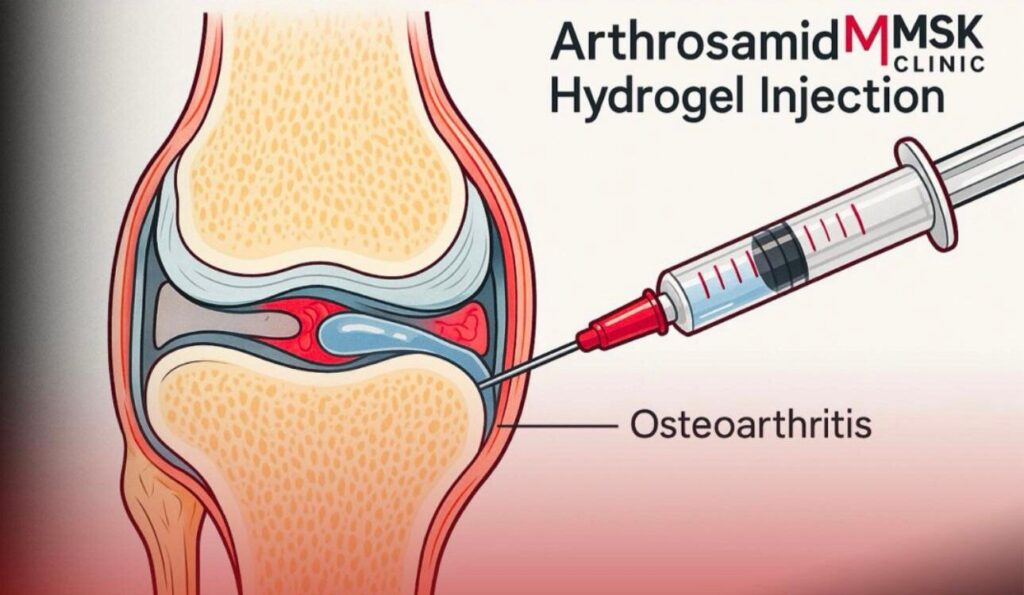
By delivering medication directly into the joint, treatments such as corticosteroids, hyaluronic acid and advanced hydrogels like Arthrosamid aim to reduce inflammation, enhance lubrication and preserve joint structure.
This targeted approach not only minimises systemic side effects but may also delay—or even prevent—the need for surgical intervention.
Purpose and Structure of This Guide
This guide offers a thorough exploration of Arthrosamid, a cutting‑edge polyacrylamide hydrogel injection designed specifically for osteoarthritis management. Readers will find clear explanations of its composition and mechanism of action, summaries of key clinical evidence, practical insights into the injection procedure and safety considerations, as well as comparisons with other injectable options.
By the end, you’ll have the evidence‑based information needed to decide whether Arthrosamid could be the right choice for your joint health journey.
Understanding Osteoarthritis (OA)
Pathophysiology: cartilage breakdown and joint inflammation
Osteoarthritis arises when the smooth, slippery cartilage that cushions the ends of bones within a joint gradually wears thin. As this protective layer deteriorates, the bones begin to rub directly against one another, triggering the release of inflammatory mediators into the joint space.
This inflammation further accelerates cartilage breakdown, in a self‑perpetuating cycle of damage.
Over time, the bone surfaces may harden (a process called subchondral sclerosis), and bony growths known as osteophytes can form at the joint margins.
Together, these changes contribute to stiffness, reduced range of motion and pain.
Common symptoms and progression stages
Early osteoarthritis often presents with intermittent joint pain after activity, mild stiffness on waking or after sitting, and slight creaking or cracking sensations (crepitus).
As the condition advances, pain may become more constant, even at rest, and joints can feel increasingly rigid.
Swelling may develop due to fluid accumulation or mild synovitis (inflammation of the joint lining).
In advanced stages, significant loss of cartilage can lead to joint deformity and marked functional impairment.
The severity of symptoms does not always correlate perfectly with imaging findings, which is why a comprehensive clinical assessment is essential.
Conventional management approaches and their limitations
First‑line strategies for osteoarthritis focus on lifestyle adjustments: maintaining a healthy weight to reduce joint load, engaging in low‑impact exercise to strengthen surrounding muscles, and using physiotherapy to improve flexibility and biomechanics.
Analgesics such as paracetamol and non‑steroidal anti‑inflammatories (NSAIDs) can offer symptom relief, while braces or orthotics may support unstable joints.
However, these measures often provide only partial or temporary benefit.
Oral medications can carry systemic side effects—particularly gastrointestinal and cardiovascular risks with prolonged NSAID use—while joint replacement surgery, though highly effective, involves significant recovery time and potential complications.
This therapeutic gap has driven interest in injectable options that target the joint directly while preserving its structure.
What Is Arthrosamid?
Definition and History of Development
Arthrosamid is an advanced intra‑articular treatment designed to alleviate symptoms of osteoarthritis by restoring joint cushioning and reducing pain.
First introduced in Denmark in the mid‑2010s, it emerged from research into polyacrylamide hydrogels—a class of materials long used in medical and cosmetic applications for their biocompatibility and stability.
Originally developed to provide a long‑lasting joint filler, Arthrosamid received CE marking (in 2021) following clinical trials that demonstrated both safety and efficacy.
Since then, it has been adopted by a growing number of specialist clinics across the UK and Europe as a minimally invasive option for patients with mild to moderate osteoarthritis who seek an alternative to traditional injectables or who wish to delay surgical intervention.
Composition: Polyacrylamide Hydrogel Properties
At its core, Arthrosamid consists of a cross‑linked network of polyacrylamide polymers suspended in a sterile aqueous solution.
This hydrogel mimics the viscoelastic properties of natural synovial fluid, providing both shock‑absorbing cushioning and smooth joint gliding.
Unlike some earlier hydrogels, the polyacrylamide matrix in Arthrosamid is non‑degradable and remains stable within the joint synovial membrane for extended periods—often two to five years
Its high water‑binding capacity helps maintain tissue hydration, while the uniform particle size ensures even distribution throughout the joint space, reducing the risk of lumpiness or uneven joint surfaces.
How Arthrosamid Differs from Other Injectables
While corticosteroids and hyaluronic acid have been mainstays of injectable osteoarthritis treatments, Arthrosamid offers several distinctive advantages.
Corticosteroids chiefly target inflammation and deliver rapid—but often short‑lived—relief, typically lasting a few weeks to months.
Hyaluronic acid supplements joint lubrication and may provide benefit for up to six months, but its effects can vary depending on formulation and patient factors.
In contrast, the polyacrylamide hydrogel in Arthrosamid serves as a semi‑permanent spacer, cushioning the joint over a much longer duration without the need for frequent repeat injections.
Furthermore, because Arthrosamid does not rely on biological molecules, it carries a lower risk of inflammatory reactions or degradation by native enzymes, offering a stable, consistent effect that can help bridge the gap between conservative therapies and eventual surgical options.
Intra‑articular Cushioning and Shock Absorption
Arthrosamid’s polyacrylamide hydrogel formulation acts as an internal buffer, restoring much of the lost cushioning within a degenerated joint. When injected, the gel fills microscopic fissures and resurfacing irregularities, creating a smooth, continuous layer that separates the opposing bone surfaces.
This viscoelastic barrier disperses mechanical loads more evenly during weight‑bearing activities such as walking or climbing stairs, thereby reducing peak stresses on focal areas of exposed bone.
Patients often report a marked reduction in grinding sensations and a more natural “give” within the joint, which translates into easier movement and less discomfort during daily tasks.
Anti‑inflammatory Effects and Pain Modulation
Although Arthrosamid does not contain pharmacological agents in the traditional sense, its presence within the joint can disrupt the cycle of cartilage wear and inflammation. By physically separating damaged surfaces, the hydrogel minimises ongoing frictional injury that would otherwise perpetuate the release of inflammatory mediators.
Moreover, the restored synovial-like environment supports healthier cellular activity in the joint lining, which can lead to reduced production of pain‑provoking cytokines.
Over time, patients may experience not only mechanical relief but also a genuine diminution in the biochemical drivers of osteoarthritic pain.
Longevity of Hydrogel Within the Joint Space
One of Arthrosamid’s most compelling attributes is its durability. Unlike hyaluronic acid preparations, which are gradually broken down by native enzymes and cleared from the joint within months, the cross‑linked polyacrylamide network remains stable for anywhere from two to five years.
Its non‑degradable nature means the gel maintains its volume and mechanical properties without the need for frequent retreatment. The material eventually becomes integrated with peri‑articular soft tissues, further anchoring it in place and ensuring consistent performance.
This lasting effect offers patients a prolonged window of symptom relief, allowing them to engage in rehabilitative exercise programmes and lifestyle modifications without recurrent flares.
Clinical Evidence & Efficacy
Key Clinical Trials and Their Outcomes
A pivotal multi‑centre study evaluated a single 6 mL Arthrosamid injection in patients with knee osteoarthritis.
At six months, participants experienced significant improvements in pain, stiffness and function, as measured by standardised osteoarthritis indices; these gains persisted at 12 months and were sustained out to two years. Three‑year follow‑up data confirmed durable pain reduction with no serious device‑related adverse events.
Comparative Studies Versus Placebo and Alternative Treatments
A systematic review of polyacrylamide hydrogels, including Arthrosamid, showed superior outcomes compared with hyaluronic acid at 52 weeks, with greater mean reductions in both pain scores and functional disability.
Although head‑to‑head randomised trials are limited, existing data suggest that Arthrosamid’s non‑degradable matrix offers more prolonged relief than biologic viscosupplements, likely due to its stable presence within the joint.
Duration of Symptom Relief and Patient Satisfaction Rates
Long‑term follow‑up indicates that most patients maintain meaningful symptom relief for up to three years after a single injection.
Over 80 per cent report improved joint comfort and daily activity levels, with high satisfaction driven by the convenience of a one‑off treatment.
Transient, mild local reactions are the most common side effect, and no long‑term safety concerns have emerged.
Indications & Patient Selection
Appropriate Osteoarthritis Grades
Arthrosamid is most suitable for individuals with mild to moderate osteoarthritis, typically corresponding to radiographic grades II and III on the Kellgren‑Lawrence scale.
At these stages, sufficient cartilage remains to benefit from the hydrogel’s cushioning effect, yet symptoms are pronounced enough to warrant intervention beyond conservative measures.
Patients with very early disease (grade I) often respond well to lifestyle modifications alone, while those with advanced, end‑stage osteoarthritis (grade IV) may require surgical options for optimal relief.
Contraindications and Cautionary Scenarios
Treatment is contraindicated in the presence of active joint infection, systemic infection or known hypersensitivity to polyacrylamide.
Arthrosamid should also be avoided in patients with significant joint deformity or instability that might impair even distribution of the gel.
Caution is advised for individuals on immunosuppressive therapy or with poorly controlled diabetes, due to elevated risks of delayed healing or local complications.
Prior joint prostheses do not categorically preclude treatment but necessitate a careful risk–benefit discussion.
Ideal Patient Profile and Shared‑Decision Making
The ideal candidate is an adult with symptomatic knee or other joint osteoarthritis unresponsive to first‑line therapies, but not yet at surgical threshold.
They should have realistic expectations about the degree and duration of symptom relief—understanding that Arthrosamid offers substantial pain reduction and improved function, but is not a cure.
A shared‑decision approach ensures that patient values, lifestyle goals and treatment priorities guide the plan.
During consultation, discussing alternative injectables, potential need for future procedures and the importance of ongoing exercise and weight management empowers patients to engage fully in their care pathway.
The Arthrosamid Injection Procedure
Pre‑injection Assessment and Imaging Requirements
Before administering Arthrosamid, a thorough clinical assessment establishes suitability and pinpoints the exact site for injection.
This typically includes a detailed history of symptoms, physical examination to assess joint range of motion and stability, and evaluation of prior treatments.
Plain radiographs (weight‑bearing X‑rays) confirm osteoarthritis grade and help exclude bone deformities or loose bodies.
In many clinics, ultrasound imaging is also performed pre‑procedure to visualise soft‑tissue anatomy, measure joint effusion and plan the optimal needle trajectory.
Routine blood tests—such as inflammatory markers and clotting profile—may be advised in patients with systemic conditions to rule out infection or bleeding risk.
Step‑by‑step: Administration under Ultrasound Guidance
- Preparation and Asepsis
The skin overlying the target joint is cleaned with antiseptic solution and draped in a sterile fashion. A high‑frequency linear ultrasound probe, enclosed in a sterile cover, is positioned to display the joint space clearly. - Local Anaesthesia
A small amount of local anaesthetic (e.g. 1% lidocaine) is injected into the skin, subcutaneous tissue and joint capsule to ensure patient comfort without distorting the joint view. - Needle Insertion
Under real‑time ultrasound guidance, a fine‑gauge needle (typically 21–22 G) is advanced into the joint synovial recess. The practitioner confirms correct needle tip placement by observing the needle shaft and bead of injected anaesthetic entering the joint space. - Hydrogel Injection
Once proper needle position is assured, the syringe containing Arthrosamid is attached. The hydrogel is injected slowly, allowing even distribution and minimising pressure spikes. Ultrasound imaging monitors dispersion of the gel, ensuring it occupies the desired joint compartments. - Needle Withdrawal and Dressing
The needle is withdrawn, and a small sterile dressing is applied. Gentle pressure is held for a minute to reduce bleeding or minor oozing.
Immediate Post‑procedure Care and Activity Recommendations
After injection, patients are observed for 10–15 minutes to monitor for any acute reactions. Mild discomfort or a feeling of joint fullness is common and typically subsides within 24–48 hours. It is advisable to:
- Rest the Joint Briefly: Avoid strenuous activities for 48 hours, but gentle range‑of‑motion exercises may commence once pain allows.
- Ice and Analgesia: Apply an ice pack for 10–15 minutes at intervals to reduce swelling; simple analgesics such as paracetamol can be used if needed (avoid NSAIDs for 48 hours unless directed).
- Gradual Return to Activity: After the initial rest period, patients are encouraged to resume low‑impact activities—such as swimming or cycling—and to follow any prescribed physiotherapy regimen to strengthen peri‑articular muscles.
- Follow‑up Appointment: A review at 4–6 weeks allows the clinician to assess response, address any concerns and plan further rehabilitation or repeat interventions if necessary.
With meticulous technique and appropriate aftercare, the Arthrosamid injection procedure offers a safe, targeted approach to managing osteoarthritis symptoms and improving joint function.
Pain Reduction and Functional Improvement Timelines
Most patients begin to notice a reduction in joint pain within two to four weeks of receiving an Arthrosamid injection.
Initial improvements are often modest, as the hydrogel integrates and begins to restore cushioning; by six to eight weeks, however, many report a substantial decline in both activity‑related and resting discomfort.
Functional gains—such as easier stair climbing or walking longer distances—typically follow closely behind pain relief, with objective measures showing meaningful improvements in joint function by three months post‑injection.
These benefits tend to plateau thereafter, providing sustained relief for up to two-three years without the need for repeat treatments.
Impact on Joint Mobility and Daily Activities
By reinstating viscoelastic support within the joint, Arthrosamid not only eases pain but also enhances range of motion.
Patients frequently describe a smoother, more natural feel when bending or extending the treated joint, with reduced stiffness on waking and after periods of inactivity.
This restored mobility enables gradual return to favourite pastimes—gardening, hill walking or gentle exercise classes—that might previously have been curtailed by discomfort. Importantly, improved joint movement also helps to break the cycle of deconditioning, as stronger muscles better support the joint and further alleviate mechanical stress.
Patient‑Reported Quality‑of‑Life Enhancements
Beyond the physical benefits, Arthrosamid has a marked positive effect on overall well‑being. Surveys conducted alongside clinical trials reveal that over 80 per cent of patients experience better sleep quality, reduced reliance on oral pain medications and greater confidence in undertaking daily tasks.
Many highlight the psychological uplift that comes with regaining independence—returning to social activities, household chores and work responsibilities with less trepidation.
These holistic gains underscore how a single, minimally invasive treatment can deliver not only symptom control but also meaningful improvements in life satisfaction.
Risks, Side Effects & Safety Profile
Common, Transient Injection‑Related Reactions
It is not unusual to experience mild, short‑lived discomfort at the injection site. Patients often report a brief sensation of pressure or fullness as the hydrogel is introduced, alongside minor redness or swelling that typically resolves within 24–48 hours.
A small proportion may feel aching or stiffness in the joint for a day or two, which can generally be managed with simple measures such as rest, gentle icing and paracetamol.
These transient effects reflect the body’s normal response to a foreign material and, in most cases, settle quickly without the need for further intervention.
Rare but Serious Adverse Events
Although Arthrosamid boasts a strong safety record, very occasional serious complications have been reported.
Deep joint infection (septic arthritis) is the most significant concern, manifesting as increasing pain, warmth, fever or reduced range of motion in the days following injection.
Immediate medical attention is essential in such instances to prevent joint damage.
Hypersensitivity reactions are exceedingly rare, given the inert nature of polyacrylamide, but any signs of widespread rash, itching or breathing difficulty warrant urgent evaluation.
Implant migration or gel displacement has been documented in isolated cases, emphasising the importance of correct injection technique under imaging guidance.
Monitoring and Reporting Safety Concerns
Vigilant follow‑up underpins a robust safety profile. Clinics should provide clear instructions on recognising warning signs and ensure a point of contact for post‑procedure concerns. A review appointment around six weeks post‑injection allows the practitioner to assess efficacy and exclude evolving complications.
If infection or another serious issue is suspected, prompt joint aspiration, laboratory analysis and, if necessary, hospital‑based treatment will be instituted.
All adverse events are reported to the relevant regulatory bodies, contributing to ongoing pharmacovigilance and refinements in best practice.
Patients are encouraged to communicate any unexpected reactions promptly, thereby safeguarding both individual care and the broader evidence base for Arthrosamid.
Corticosteroids: Rapid Relief Versus Duration of Effect
Corticosteroid injections are renowned for their swift and potent anti‑inflammatory action, often delivering noticeable pain relief within hours to days. By suppressing inflammatory mediators in the joint lining, they can dramatically reduce swelling and stiffness.
However, this benefit typically peaks around one to two weeks post‑injection and then gradually wanes, with effects commonly lasting three to six months. Repeated courses may risk cartilage thinning and systemic side effects, so their use is generally limited to episodic flares rather than long‑term management.
Hyaluronic Acid: Viscosupplementation Differences
Hyaluronic acid injectables aim to restore the natural viscoelasticity of synovial fluid, enhancing lubrication and shock absorption. Unlike corticosteroids, they work more slowly—patients often notice improvement over several weeks—and the duration of symptom relief tends to extend to six months or longer, depending on the specific formulation. Because hyaluronic acid is a naturally occurring molecule, the risk of adverse reactions is low, but enzymatic breakdown within the joint necessitates repeat treatments every six to 12 months to maintain benefit.
Emerging Biologics (PRP, Stem Cells) Versus Hydrogel
Biologic therapies such as platelet‑rich plasma (PRP) and mesenchymal stem cell injections seek to harness the body’s own healing mechanisms. PRP delivers concentrated growth factors to promote tissue repair, while stem cells may differentiate into cartilage‑like cells and secrete anti‑inflammatory cytokines.
Early studies report promising improvements in pain and function, yet standardisation of preparation methods and long‑term efficacy data remain limited.
In contrast, hydrogel injections like Arthrosamid offer a consistent, stable mechanical solution without relying on patient‑derived materials, providing predictable cushioning and a well‑established safety profile.
While biologics hold potential for regenerative benefit, hydrogels excel in delivering durable symptom control with a single treatment.
Cost Considerations & Funding Options
Typical Price Range per Injection in the UK
A single Arthrosamid injection generally costs between £2,500-3000, though fees vary by clinic location and whether ultrasound guidance or follow‑up consultations are bundled into the package
Private Pay Versus Insurance Coverage
Arthrosamid is regarded as an elective, self‑funded therapy. Most private health insurers in the UK do not cover polyacrylamide hydrogel injections for osteoarthritis, so patients should be prepared to meet the full cost out of pocket.
Value Analysis: Cost per Quality‑Adjusted Life Year
Health‑economic assessments use the incremental cost‑effectiveness ratio (ICER) to compare treatments by their cost per quality‑adjusted life year (QALY) gained. The recognised threshold range for cost effectiveness in the UK is £20,000–£30,000
- If a £3,000 injection of Arthrosamid delivers a utility gain of 0.1 QALY per year over two years (total 0.2 QALY), the cost per QALY would be £15,000 (£3,000 ÷ 0.2 QALY), well below the lower NICE threshold.
- This suggests Arthrosamid represents strong value for money compared with repeated short‑duration injectables and even some surgical interventions, by offering durable symptom relief at an acceptable ICER.
Patient Testimonials & Case Studies
Real‑world Success Stories
“I was sceptical at first, but within six weeks of my Arthrosamid injection I noticed a real difference,” recalls Sarah, a 62‑year‑old retired teacher with moderate knee osteoarthritis. “Walking the dogs used to be a painful chore; now I can cover over a mile without stopping.” Mark, aged 55 and an avid cyclist, experienced similar relief in his wrist joint: “I’d given up on weekend rides because of throbbing pain, but two months post‑injection I was back on my bike, pain‑free.” These accounts reflect the experiences of many patients who choose Arthrosamid to regain mobility and return to activities they love.
Before‑and‑After Functional Assessments
Objective measures often mirror patient reports. In one case series, average knee flexion improved from 100° to 120° at three months, while timed up‑and‑go tests decreased from 14 seconds to 10 seconds, signalling easier transitions from sitting to walking.
Lessons Learned and Tips for New Patients
Preparation and realistic expectations are key. Patients benefit from discussing goals with their clinician—whether that’s resuming particular sports or simply walking without analgesics.
Gentle physiotherapy started four weeks after injection helps consolidate gains, so engaging with a tailored exercise programme is highly recommended.
Many find keeping a diary of symptoms useful to track progress and guide follow‑up.
Finally, maintaining a healthy body weight and avoiding high‑impact activities in the early post‑procedure period reduces the risk of flare‑ups, setting the stage for long‑term success with Arthrosamid.
My MSK Clinic’s Arthrosamid Service (Manchester)
At our Deansgate clinic, Consultant Physiotherapist Amir Akhtar leads a dedicated team offering precision, ultrasound‑guided Arthrosamid injections for knee and other joint osteoarthritis. Priced at £2,995 (including consultation, imaging and Antibiotics), each treatment is delivered in a comfortable, modern suite just a short walk from Manchester Piccadilly.
FAQs
How is Arthrosamid administered differently from other injectables?
Arthrosamid is delivered via a single injection under ultrasound guidance, ensuring precise placement of the hydrogel. Unlike some treatments that require multiple weekly injections, Arthrosamid’s non‑degradable matrix typically necessitates only one procedure for long‑term effect.
Which joints can be treated with Arthrosamid?
While most experience has been in the knee, Arthrosamid has also been used successfully in other synovial joints—such as the hip, ankle, shoulder and wrist—provided there is sufficient remaining cartilage.
Do I need any special preparation before the injection?
Patients should avoid anti‑inflammatory medications (NSAIDs) for 48 hours beforehand and refrain from vigorous exercise on the day of treatment. A light meal is advisable, and any routine blood tests or imaging studies should be completed in advance as instructed by your clinic.
Can Arthrosamid be combined with other therapies?
Yes. Many clinicians recommend a multimodal approach—combining Arthrosamid with a tailored physiotherapy programme, weight‑management strategies and, when appropriate, supplementary treatments such as low‑dose corticosteroid or hyaluronic acid injections in different treatment windows.
How much downtime should I expect?
Downtime is minimal. Aside from resting the joint for the first day, most patients return to normal light activities within 48 hours. High‑impact sports should be paused for 2 weeks, or until your physiotherapist advises you’re ready.